Simulation of Electric Stimulation for Bone Growth
Collaborating Investigators: Roy Bloebaum, Brad Isaacson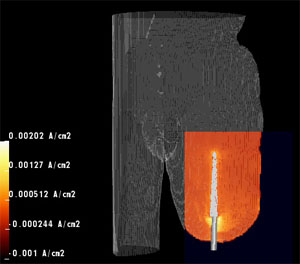 The Center is working closely with scientists at the VA Bone and Joint Research Lab to improve the success of prosthetic limb implants for injured combat veterans. For surgeons installing artificial metal implants that connect directly to bone, a major challenge is achieving good osseointegration, the bond between the living bone and the surface of the load bearing implant. Osseointegration is achieved by encouraging the bone to grow into the artificial material, creating a strong skeletal interlock.1,2 This form of prosthetic attachment has major advantages over traditional stump and socket, especially in the population of combat veterans who have lost limbs from explosive devices and typically have little residual limb length left to attach the prosthesis. Control of bone growth, or osseogenesis, at the interface site is essential for achieving rapid and successful osseointegration.
The Center is working closely with scientists at the VA Bone and Joint Research Lab to improve the success of prosthetic limb implants for injured combat veterans. For surgeons installing artificial metal implants that connect directly to bone, a major challenge is achieving good osseointegration, the bond between the living bone and the surface of the load bearing implant. Osseointegration is achieved by encouraging the bone to grow into the artificial material, creating a strong skeletal interlock.1,2 This form of prosthetic attachment has major advantages over traditional stump and socket, especially in the population of combat veterans who have lost limbs from explosive devices and typically have little residual limb length left to attach the prosthesis. Control of bone growth, or osseogenesis, at the interface site is essential for achieving rapid and successful osseointegration.
Current methods for promoting osseointegration involve placing a load on the prosthesis for extended periods of time, which encourages osseogenesis at the implant interface.3 However, this method is not always successful and osseointegration remains a challenge. The Center collaborates with Professor Roy Bloebaum and his team at the VA Bone and Joint Research Lab to develop new methods for promoting osseogenesis using electrical stimulation and to improve the technology for achieving rapid, quality osseointegration in veterans with combat related injuries.4,5
The goal of this project is to develop an Osseointegrated Intelligent Implant Design (OIID) system, a comprehensive and validated computational infrastructure that will support the creation of patient specific models of the residual limbs of amputees to assist in the evaluation and treatment by means of osseointegration. The Center will provide specially adapted software required for many aspects of this system including image based modeling, visualization, simulation, and estimation. Seg3D, for example, will identify from CT scans the tissues that make up the residual limb. Then with BioMesh3D, investigators can generate patient specific geometric models that will be the basis for simulations of electric field from selected stimulating electrode configurations using the SCIRun problem solving environment. Comparison of simulated results to measured results in patients will provide validation and allow further refinement of the simulation. This research will result in a system for quickly assessing optimal electrode placement for electrically enhanced osseointegrated implants. Development of the OIID system will be of great benefit to our injured combat veterans and will likely lead to other applications that require osseointegration.
[1] T. Albrektsson and C. Johansson. Osteoinduction, osteoconduction and osseointegration. Eur Spine J,
10 Suppl 2:S96–101, 2001.
[2] R. D. Bloebaum, J. P. Beck, R. Olsen, L. Norlund, and K. N. Bachus. Development of a single stage surgical model for percutaneous osseointegrated implants for amputees. In 55th Annual Meeting of the Orthopaedic Research Society, volume 34, page 2255, Las Vegas, NV, 2009.
[3] A.A. Hofmann, R.D. Bloebaum, and K.N. Bachus. Progression of human bone ingrowth into porouscoated implants. Acta Orthop. Scand., 68(2):161–166, 1997.
[4] Z. B. Friedenberg, L. M. Zemsky, R. P. Pollis, and C. T. Brighton. The response of non-traumatized bone to direct current. J Bone Joint Surg Am, 56(5):1023–30, 1974.
[5] C. T. Brighton. The treatment of non-unions with electricity. J Bone Joint Surg Am, 63(5):847–51, 1981.