Tutorial Sample
Tray 1
Body Fluid Examples
Objectives
After reviewing this tray (assignment), you should be able to:
1. List laboratory procedures and features that distinguish transudates from exudates. 2. Distinguish mesothelial cells from macrophages and monocytes, as well as tumor cells. 3. Recognize calcium pyrophosphate and monosodium urate crystals with polarized compensated light microscopy. 4. Recognize tumor cells in body fluids. 5. Recognize bacteria in body fluids. 6. Distinguish reactive lymphocytoses from lymphoma and leukemia in fluids.
Instructions
1. Suggested Readings: A. Body Fluids, Third Edition, Kjeldsberg CR, and Knight J eds, ASCP Press, Chicago, 1993. B. Henry’s Clinical Diagnosis and Management by Laboratory Methods, 21st Edition, Chapter 28, McPherson R, Pincus M, eds, Saunders Elsevier, Philadelphia, 2007. C. Color Atlas of Hematology: Glassey EF eds. CAP Press, Northfield, IL, 1998. 2. There are no histories for this tray of slides. 3. This tray contains different examples of Wright stained body fluids. Look at these slides "cold". Write down the most likely diagnosis and then look at the answers. 4. Make notes of any questions you may have and review the tray with the hematopathology faculty or fellows. 5. Take the self-assessment written exam for Tray 1 and discuss any questions with the hematopathology fellows or attending.
Comment Sheet
Body Fluids
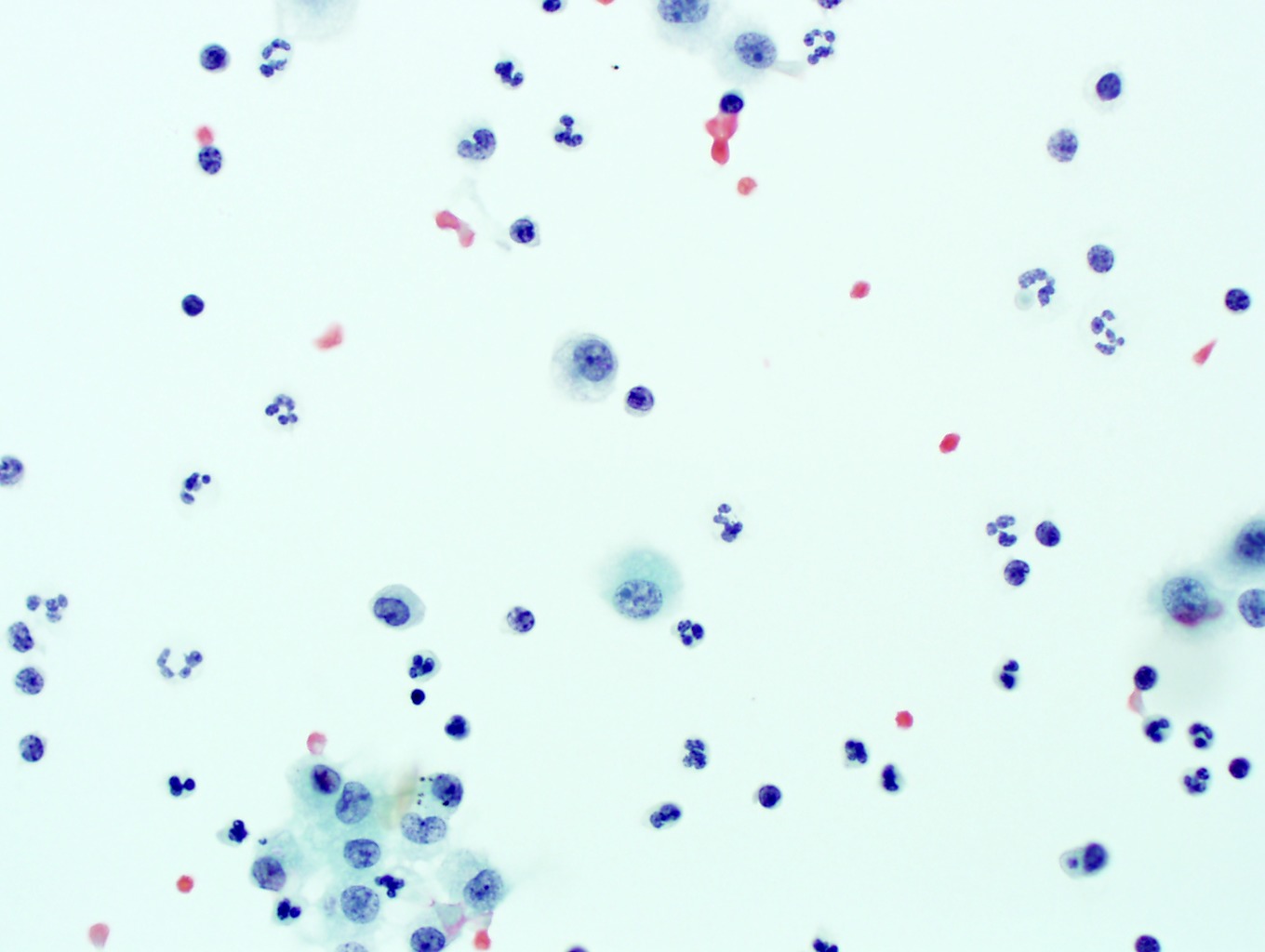
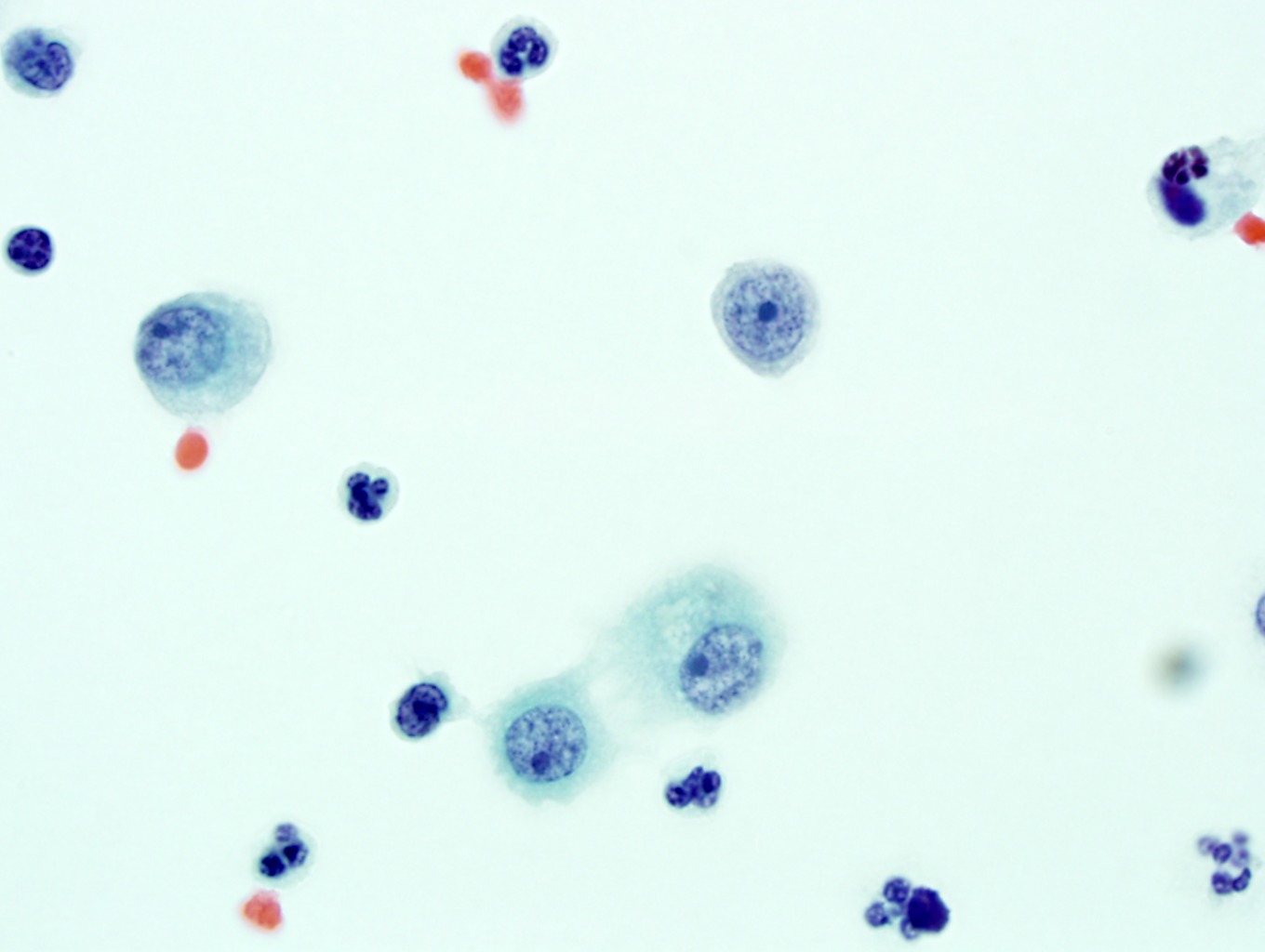
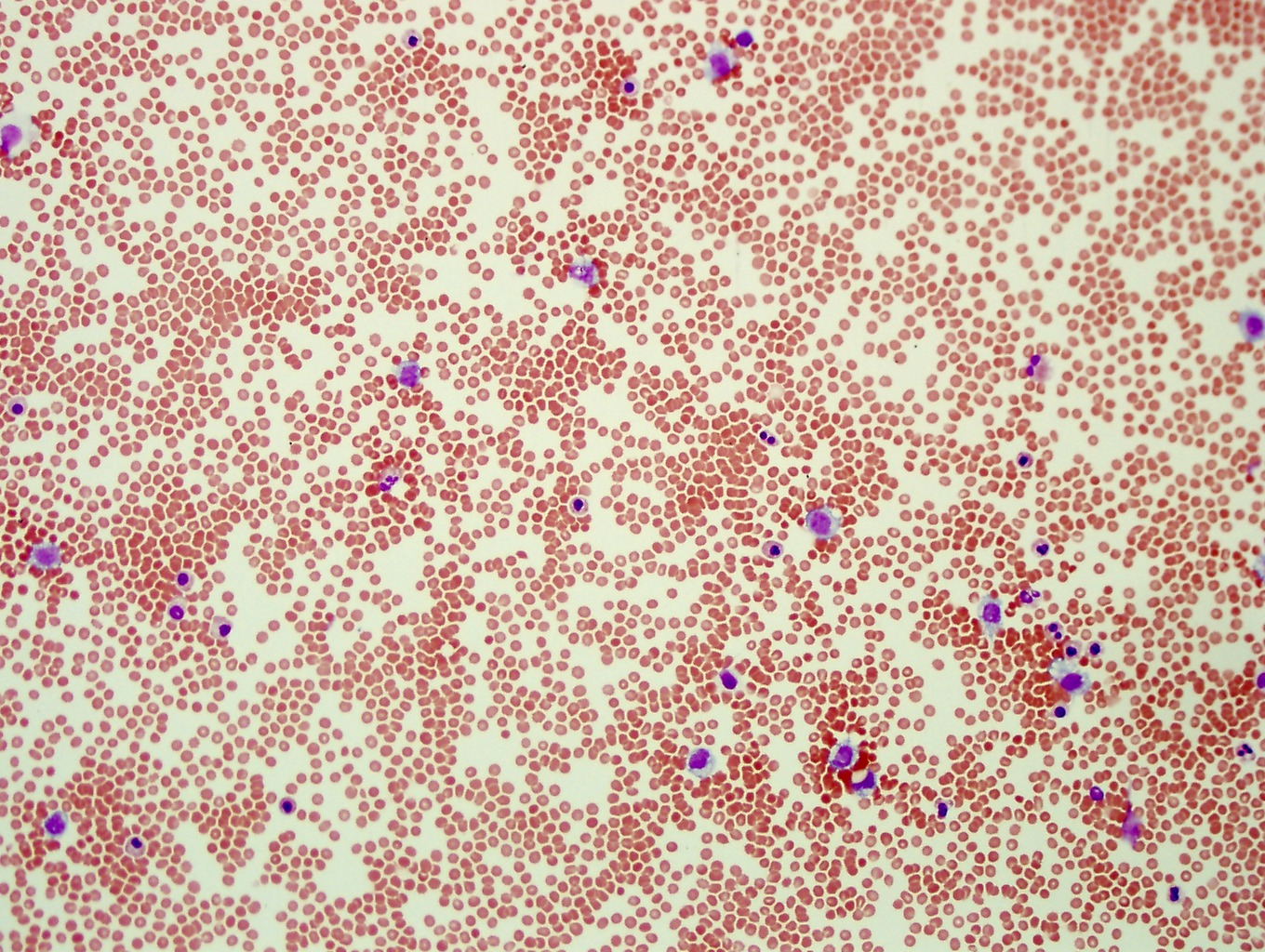
1. This is not a very good Wright stain on a cytocentrifuge preparation from a pleural fluid. Unfortunately, not all specimens you will end up having to review are going to be properly stained. It is important to recognize that there are no abnormal cells present on this preparation. Any unusual morphology is due to the quality of the stain. If possible, another sample should be restained. Image 1-1, Image 1-2, Image 1-3
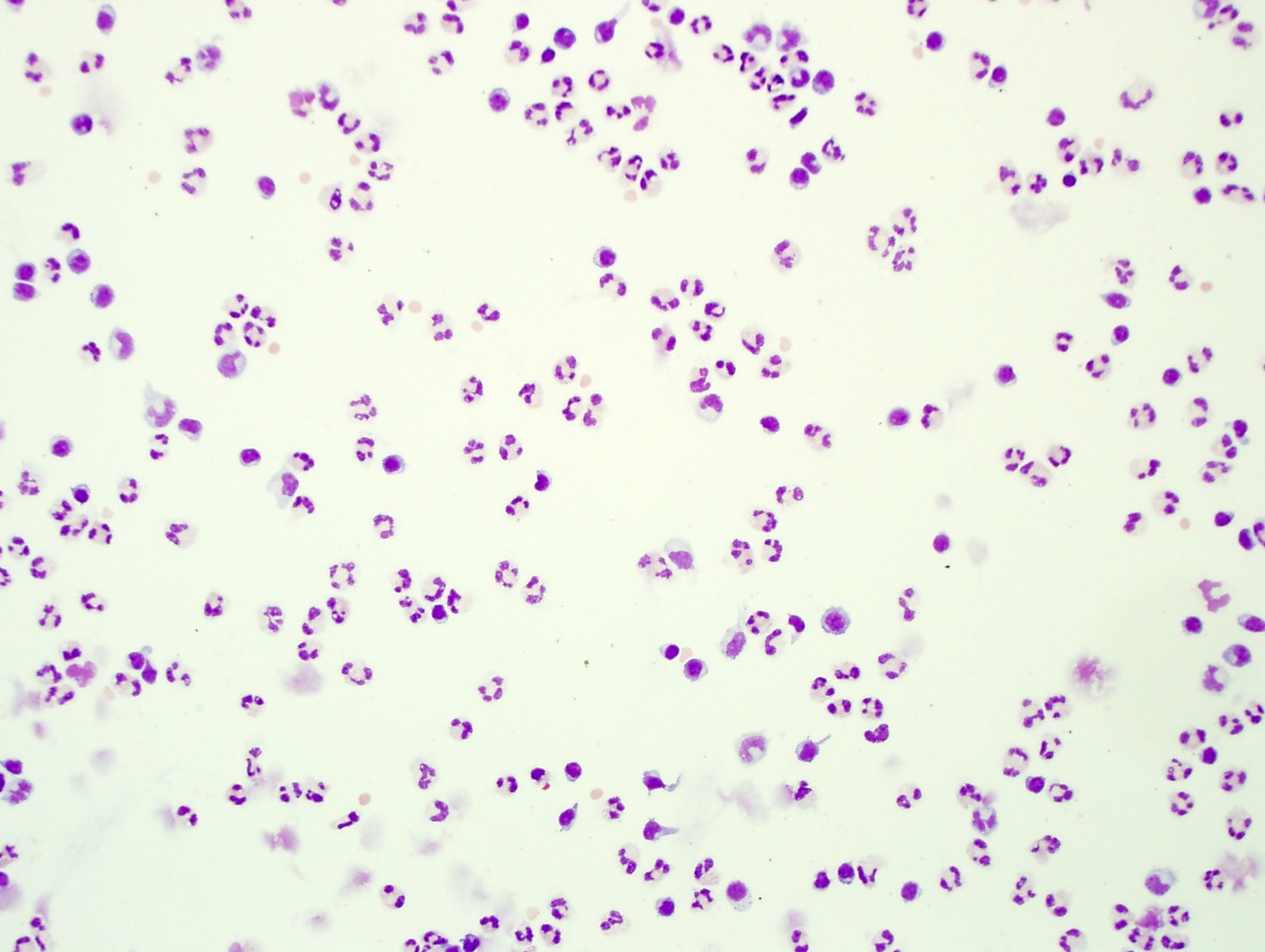
2. This pleural fluid is extremely cellular. Note the numerous eosinophils and a few admixed neutrophils. Very carefully look at the individual cells and make sure you can distinguish neutrophilic granulocytes from eosinophils. The neutrophils have finer granules and usually greater than two nuclear segments where as eosinophils will have coarser granules which are often orange-red in color and the nucleus is usually bilobed. Eosinophilic pleural effusions are often idiopathic but can be seen with pneumothorax, infection, hypersensitivity states, autoimmune disorders and associated malignancy. Image 1-4, Image 1-5, Image 1-6
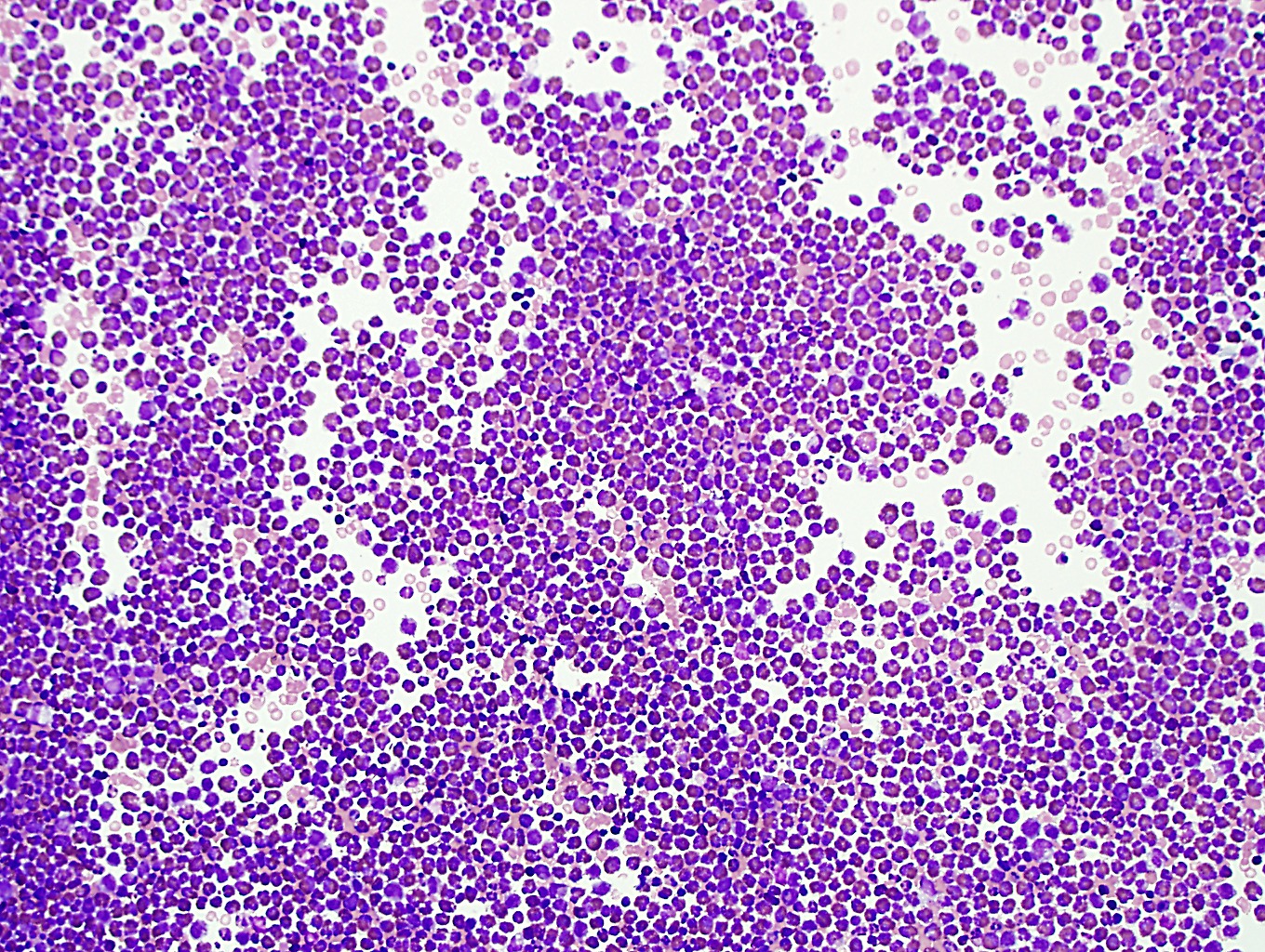
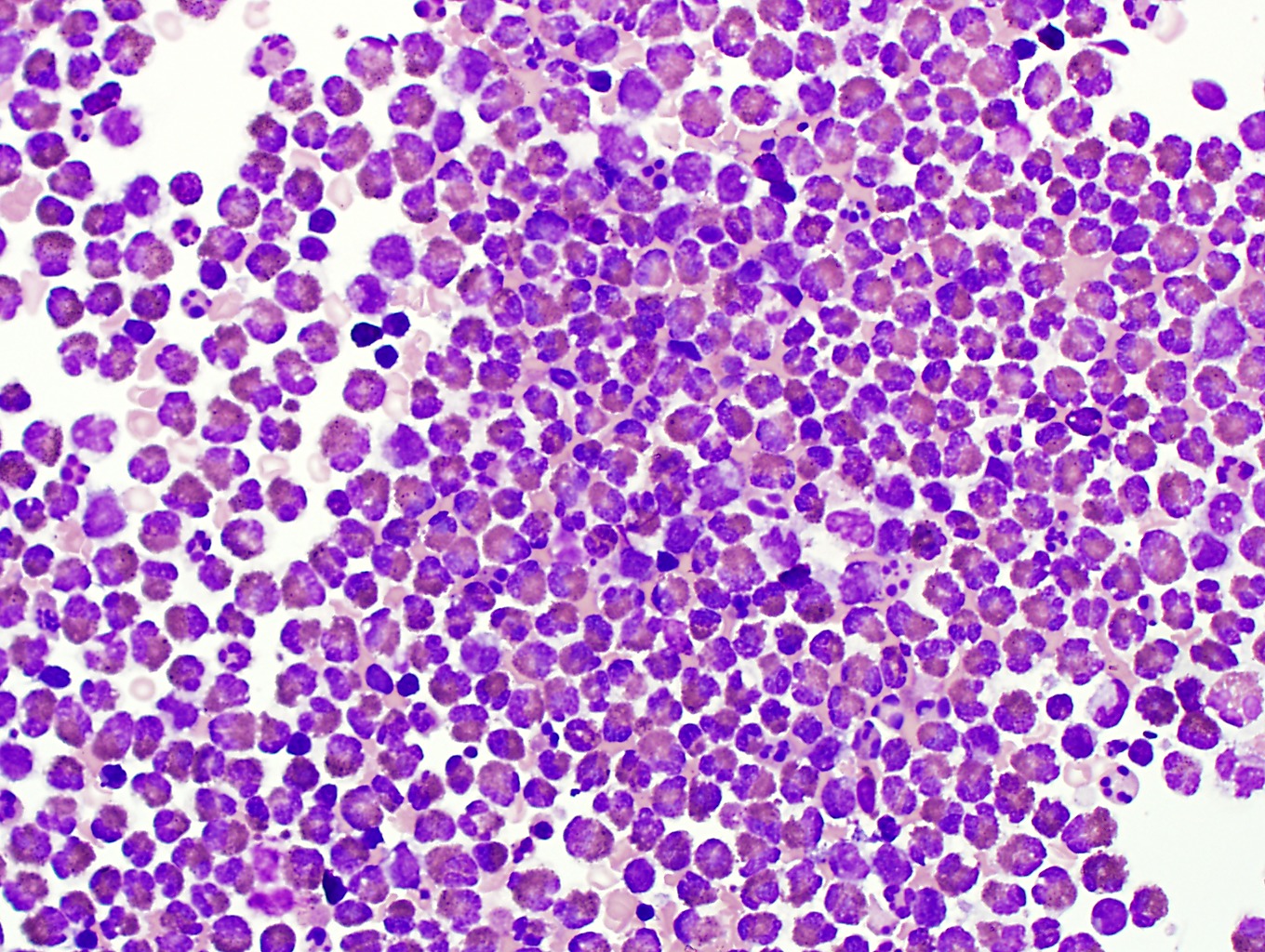
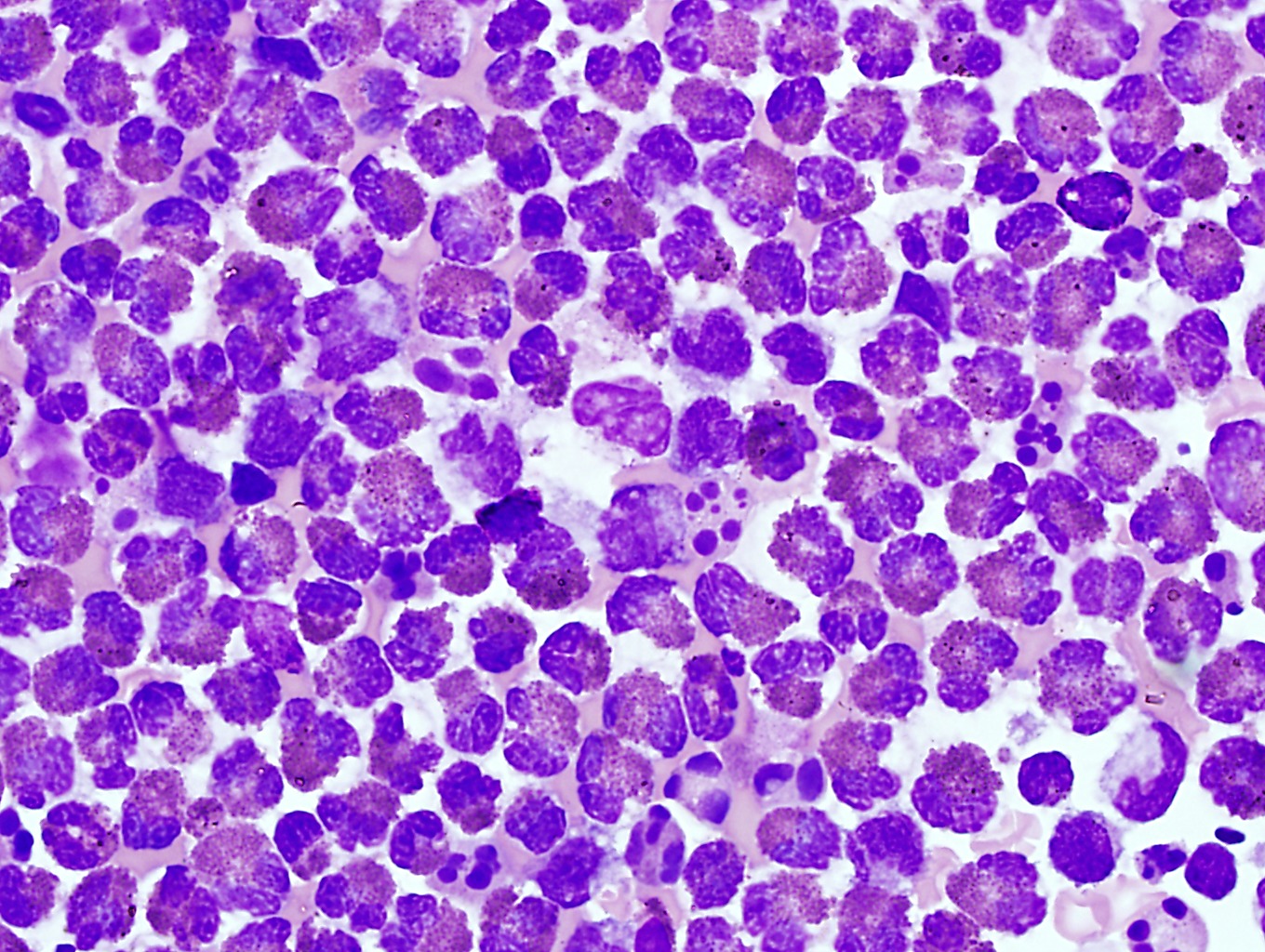
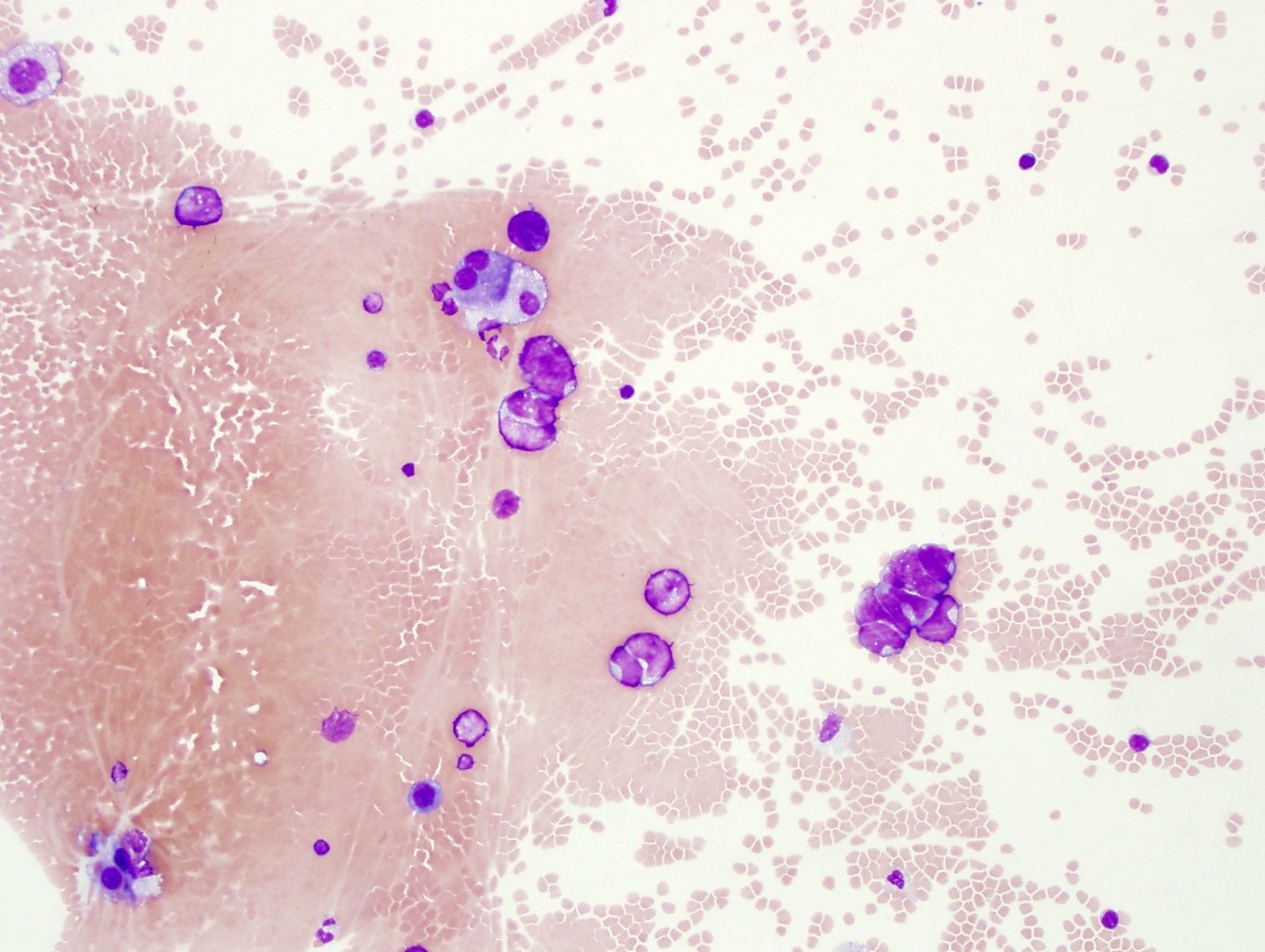
3. This pleural fluid contains lymphoma. Note the large size and irregular nuclear contours. Some of the lymphoma cells have nucleoli. Remember that the subclassification of lymphomas is typically based on histologic examination of a lymph node and not on the morphological features of cells in body fluids. The lymphoma cells are seen individually and not as clumps or clusters typical of carcinoma. The discohesive nature of these cells and their large size compared to reactive lymphocytes are features of lymphoma. Flow cytometry immunophenotyping can often, but not always, provide information on the expression pattern of the lymphoma. Image 1-7, Image 1-8, Image 1-9
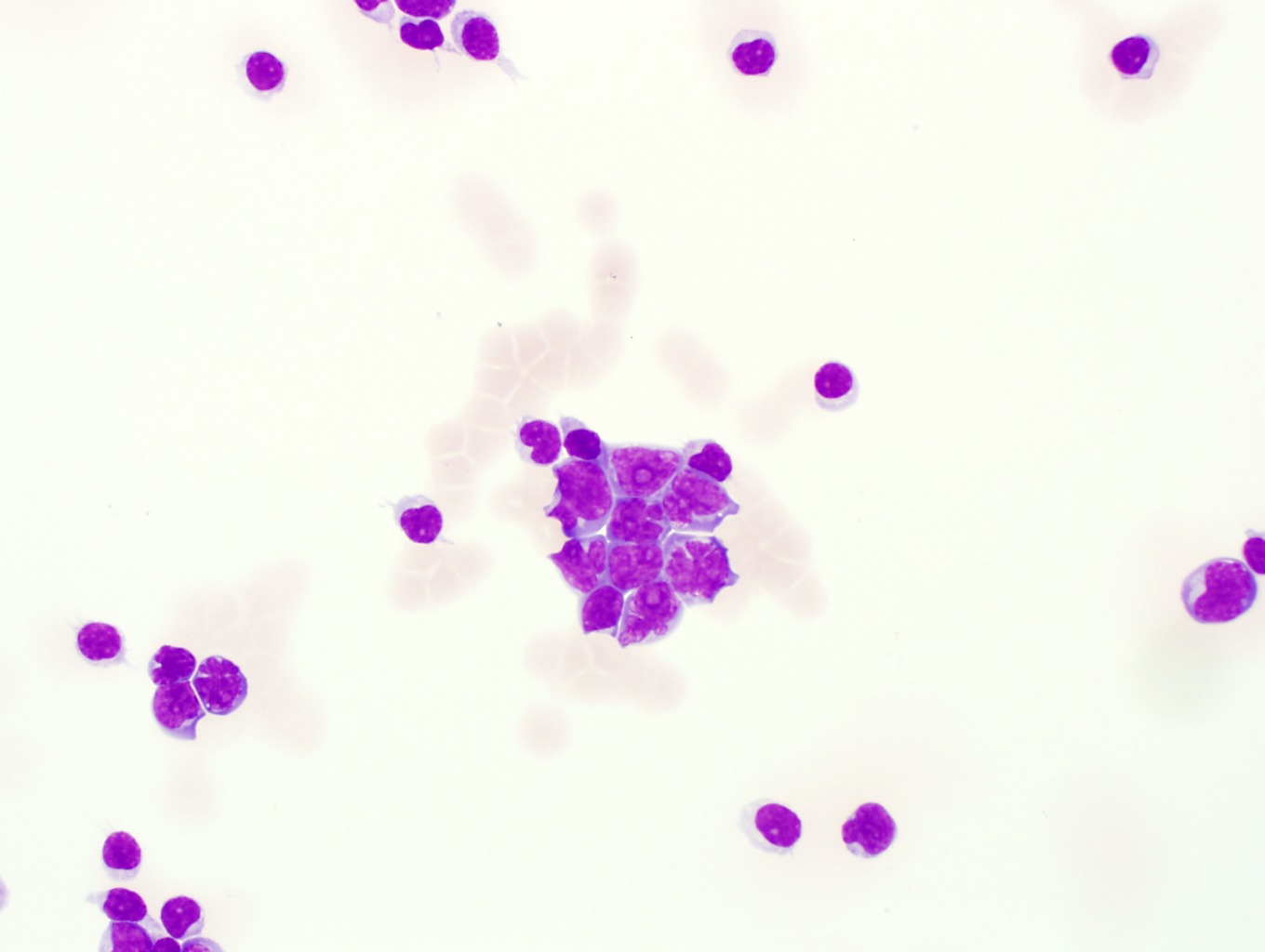
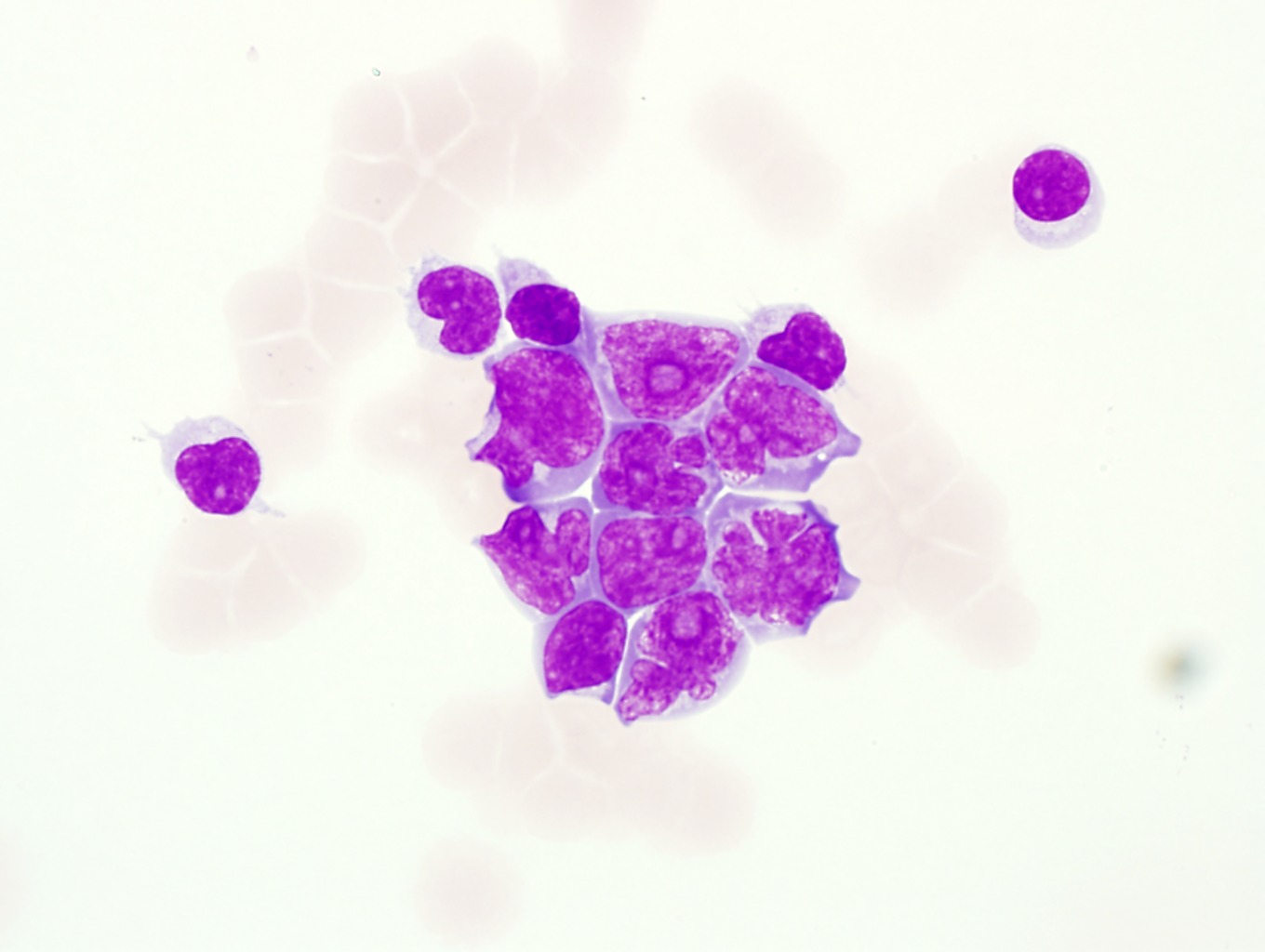
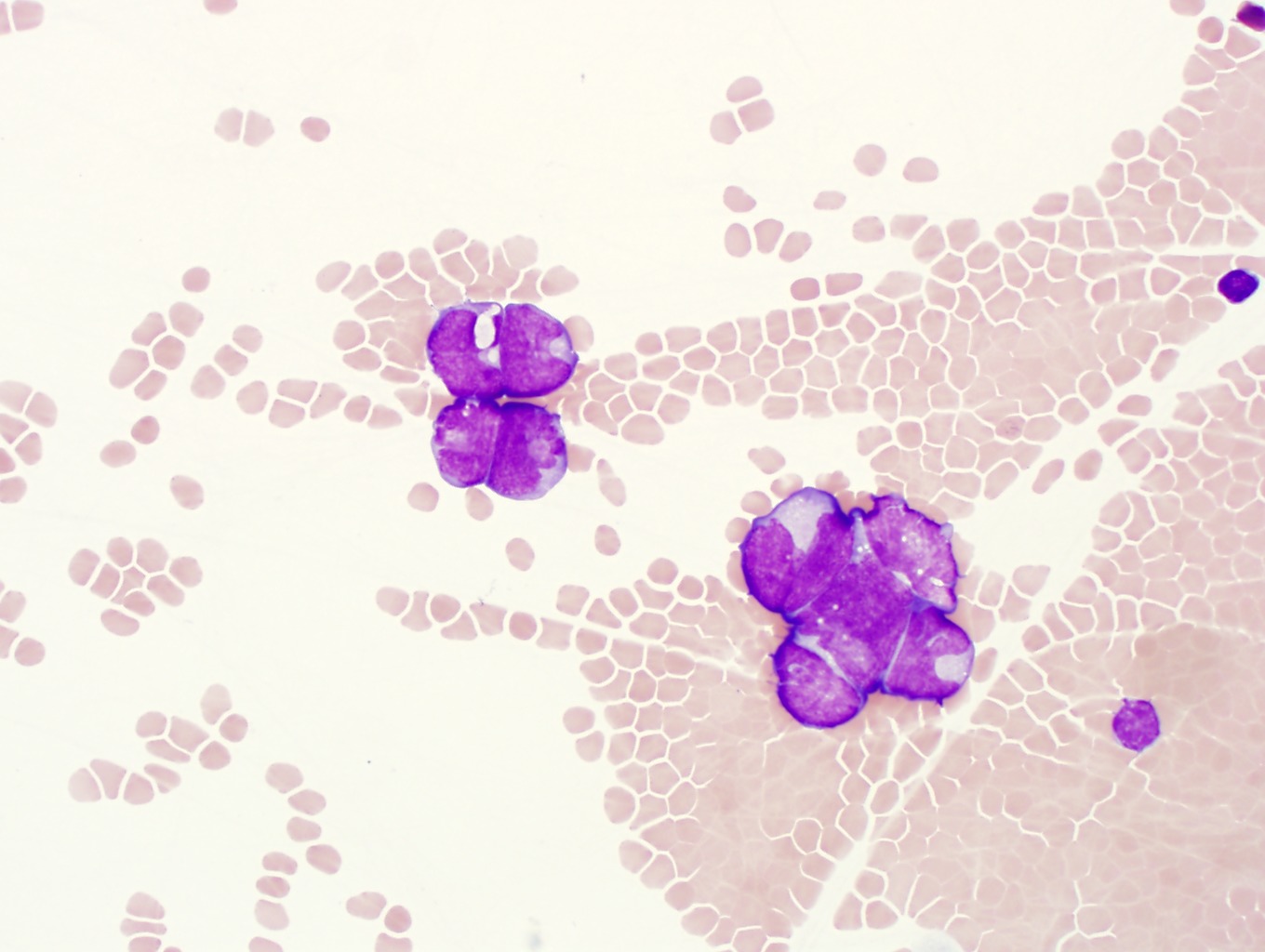
4. This pleural fluid (Wright stain) contains carcinoma. Note the large clumps of cohesive cells with nuclear molding, variably abundant cytoplasm and occasional prominent nucleoli suggestive of metastatic cancinoma. Compare the size of these cells to the background neutrophils, lymphocytes and monocytes. Immunohistochemical staining may be helpful to distinguish mesothelial cells (reactive or neoplastic) from metastatic carcinoma or other cell types. Image 1-10, Image 1-11, Image 1-12
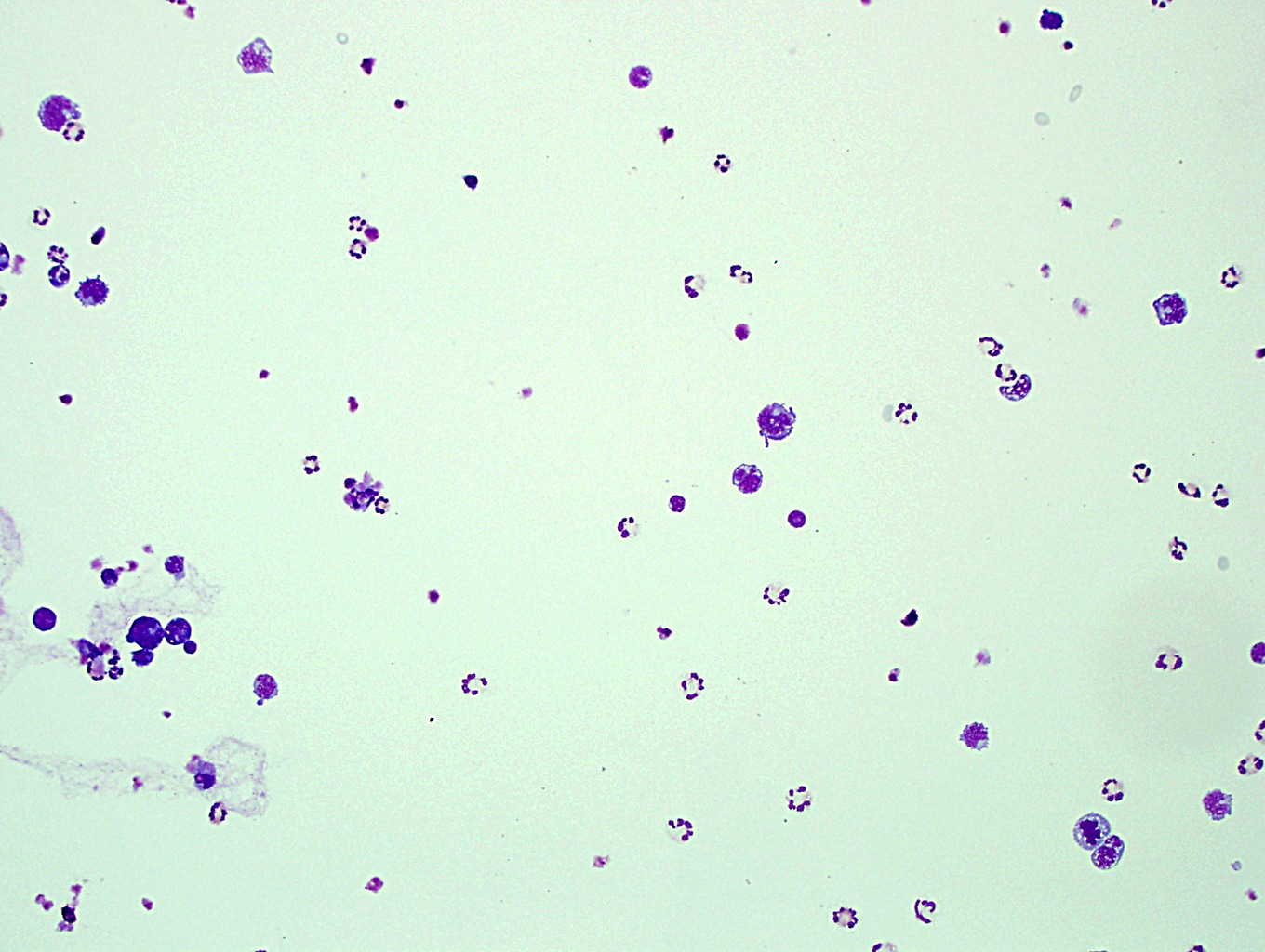
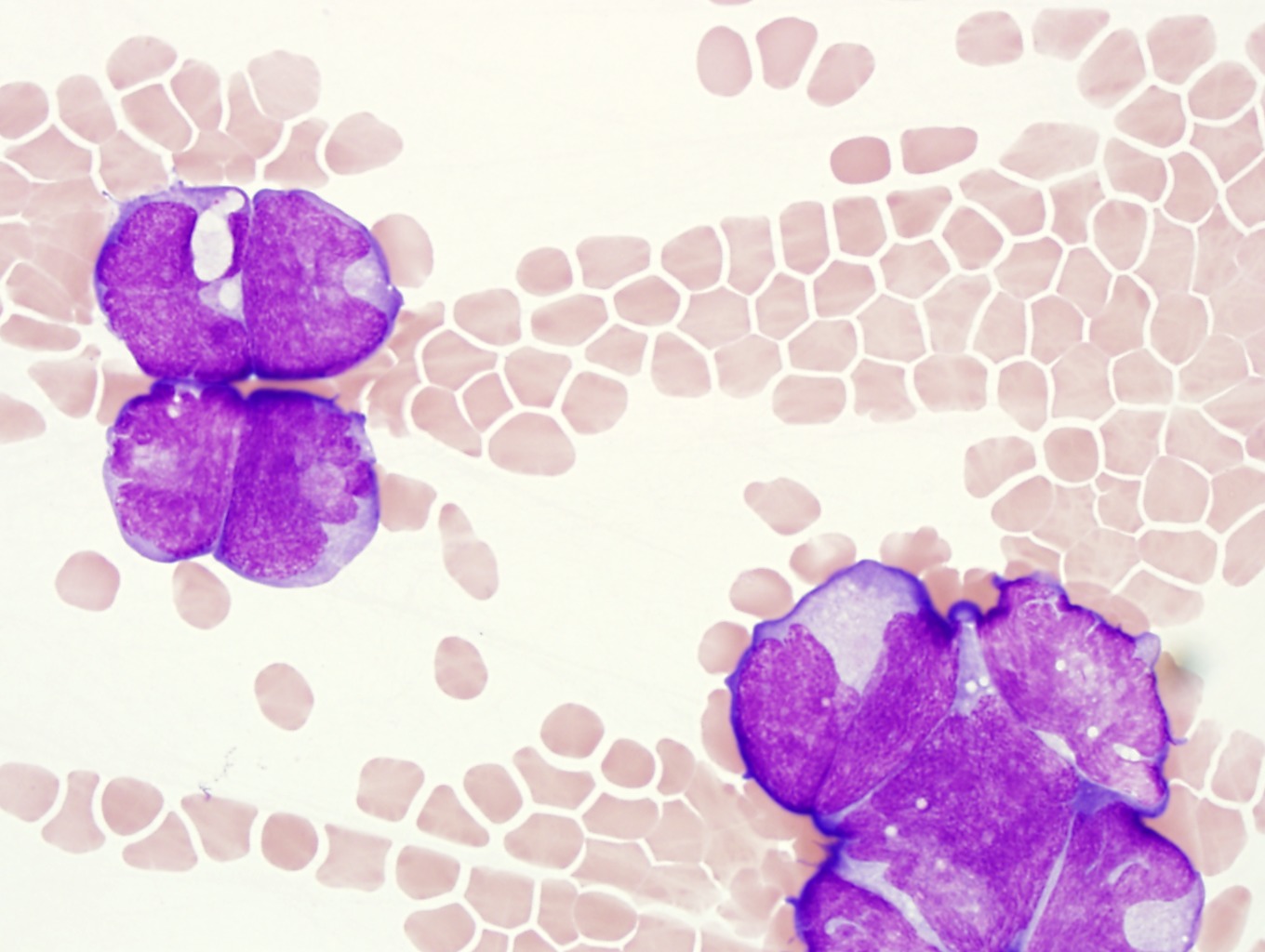
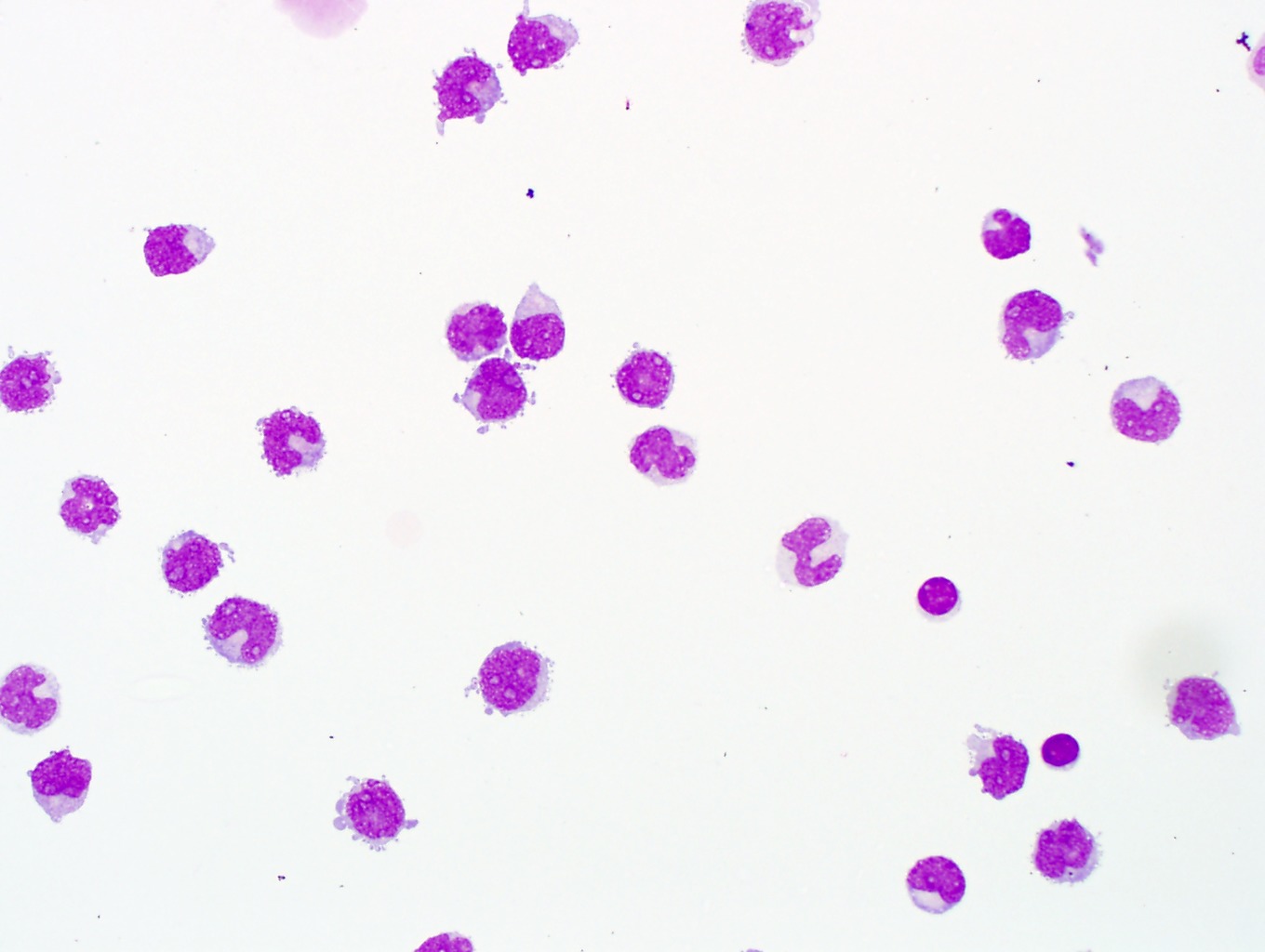
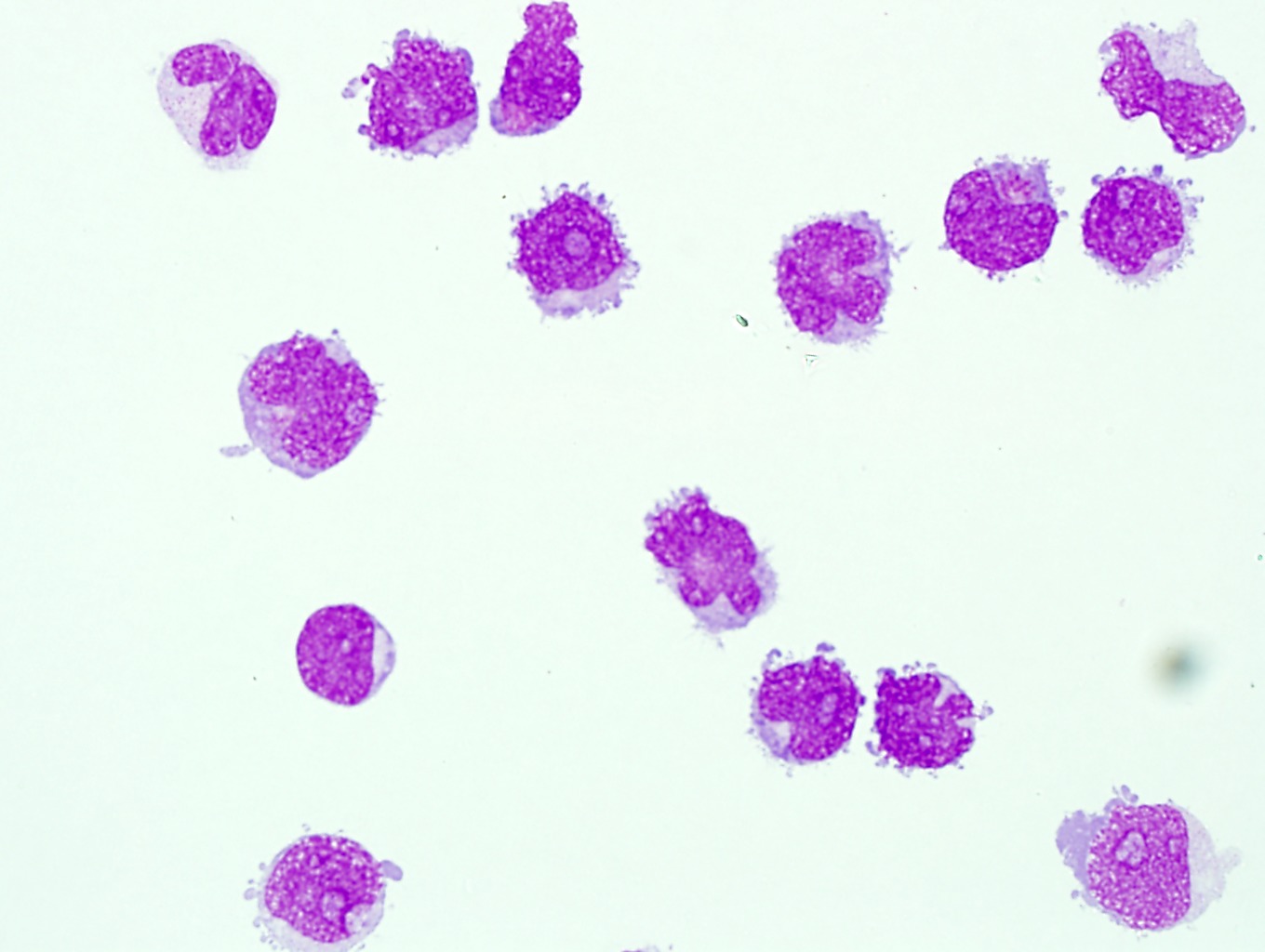
5. This pleural fluid also contains lymphoma. Note the large size of the lymphoma cells. Many of them have high nuclear:cytoplasmic ratios, irregular nuclear contours, and prominent nucleoli. Overall, these cells are very similar (monotonous) in appearance, have grey to basophilic cytoplasm with no granules, and are too large to be normal reactive lymphocytes. A reactive infiltrate should show a spectrum of cell sizes and differentiation. Image 1-13, Image 1-14, Image 1-15
6. These pleural fluids contain reactive mesothelial cells with atypia (A and B). Mesothelial cells may contain multiple nuclei as in this preparation, which may cause concern for malignancy. Some also appear to contain intracytoplasmic vacuoles. Careful attention to the spectrum of the mesothelial cells is helpful. Some cases will require immunohistochemical staining to exclude a neoplasm. Clinical history is also important. (Image 1-16, Image 1-17, Image 1-18 for A) and (Image 1-19, Image 1-20, Image 1-21 for B)
7. This peritoneal fluid (Wright stain) contains malignant cells. In malignant effusions and with mesothelial cell atypia, the Wright stain often over-stains the cells so that nuclear features are difficult to interpret. Additional studies, such as immunohistochemical staining may be needed to distinguish the malignant cell population. Image 1-22, Image 1-23, Image 1-24
8. A. Peritoneal fluid with malignant cells (Papanicolaou stain). This represents ovarian carcinoma. B. Pleural fluid with atypical mesothelial cells. These slides exemplify how helpful the Papanicolaou stain can be for distinguishing nuclear features that allow you to distinguish between reactive and malignant process. Also note the cohesiveness of the cells and the numerous mitoses in slide A. (Image 1-25, Image 1-26, Image 1-27 for A) and (Image 1-28, Image 1-29, Image 1-30 for B)
9. This is a pleural fluid with malignant cells present. Hidden amongst the mesothelial cells and histiocytes there are a few large malignant cells. This patient has a history of Hodgkin lymphoma. It would be difficult to identify the origin of these cells and whether or not they are definitively malignant on morphology alone. However, this slide illustrates how important it is to scan the slide under low power so that small numbers malignant cells are not missed. Image 1-31, Image 1-32, Image 1-33
10. This is an example of CSF with hemorrhage. This case does not show the presence of hemosiderin pigment, indicating it was a recent bleed. Note the degenerating neutrophils with condensed and pyknotic nuclei which could be mistaken for nucleated RBC's. Image 1-34, Image 1-35, Image 1-36
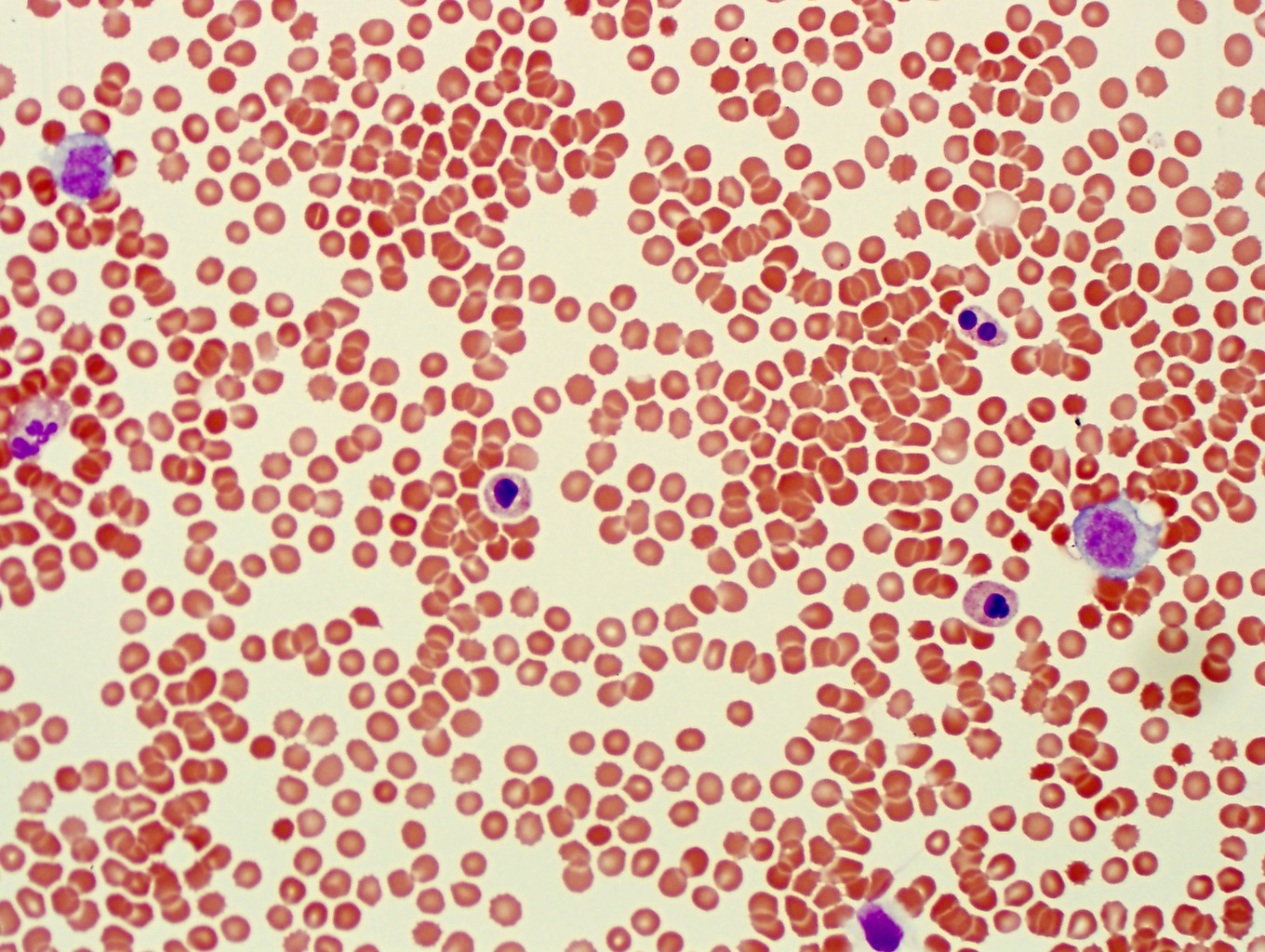
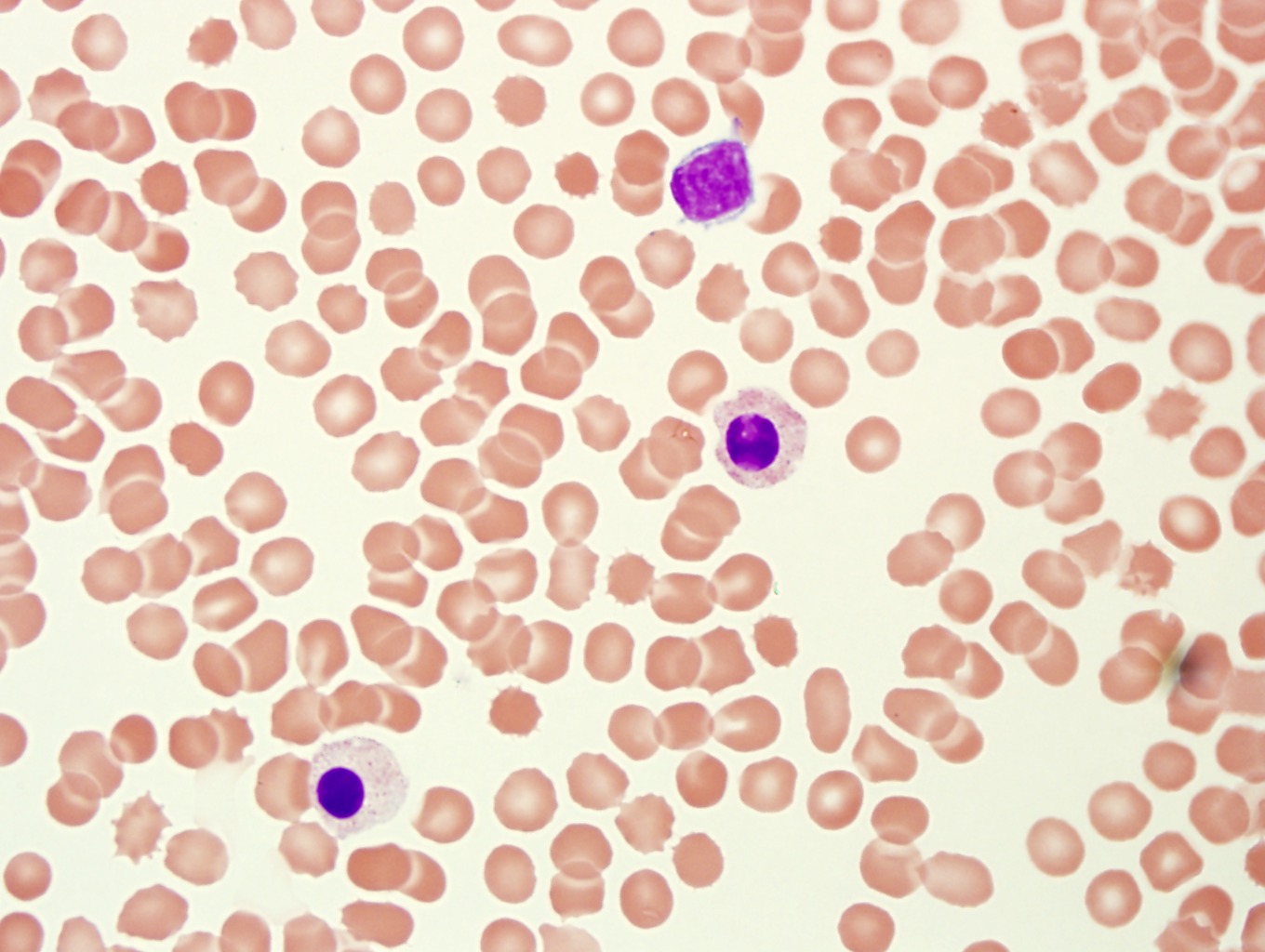
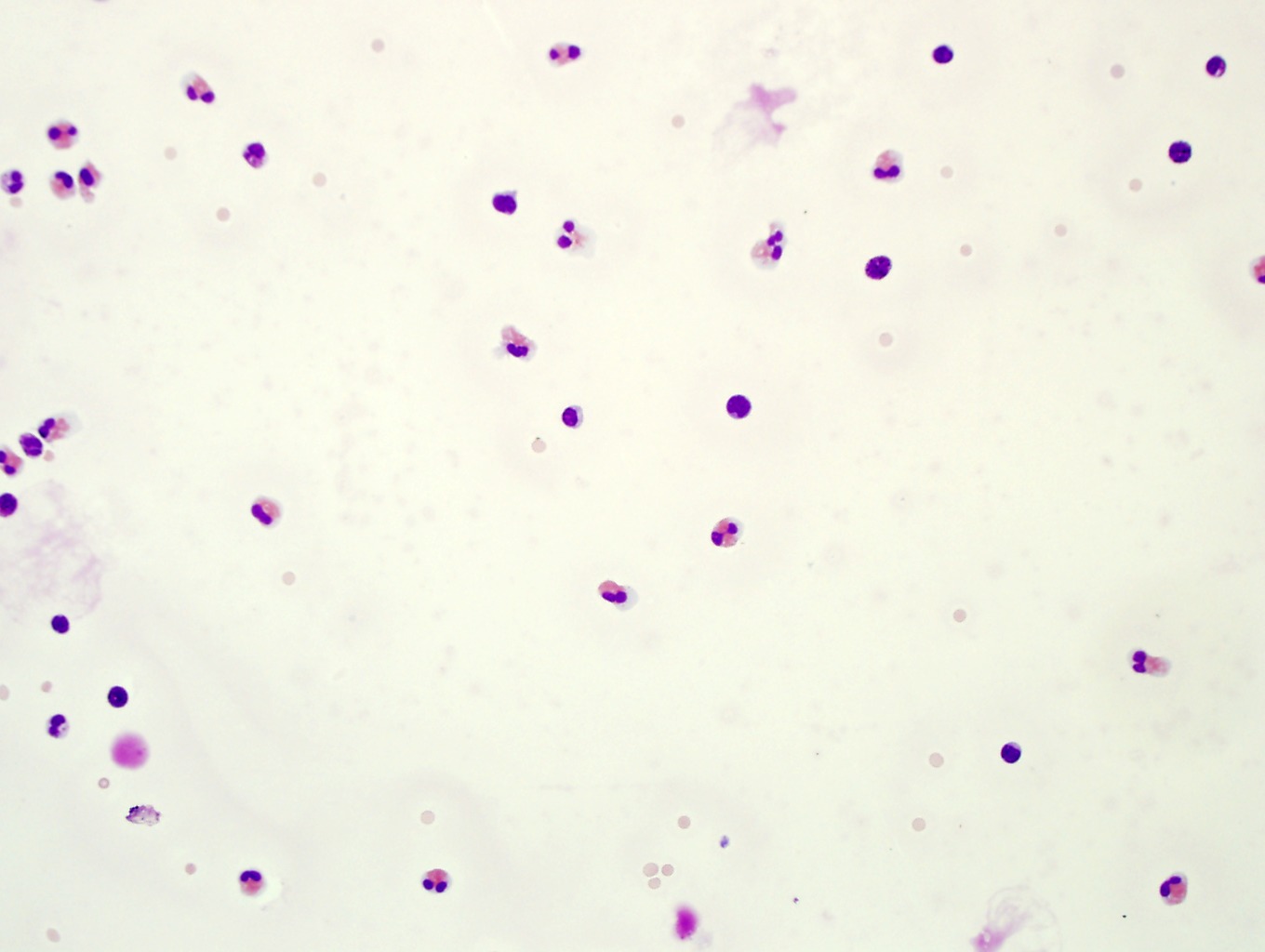
11. This CSF contains rare blasts. You missed this case if you did not see the blasts that are present. Note the fine chromatin and high N/C ratios in the blasts. This patient has a history of ALL with eosinophilia. Many basophils are also present. Image 1-37, Image 1-38, Image 1-39
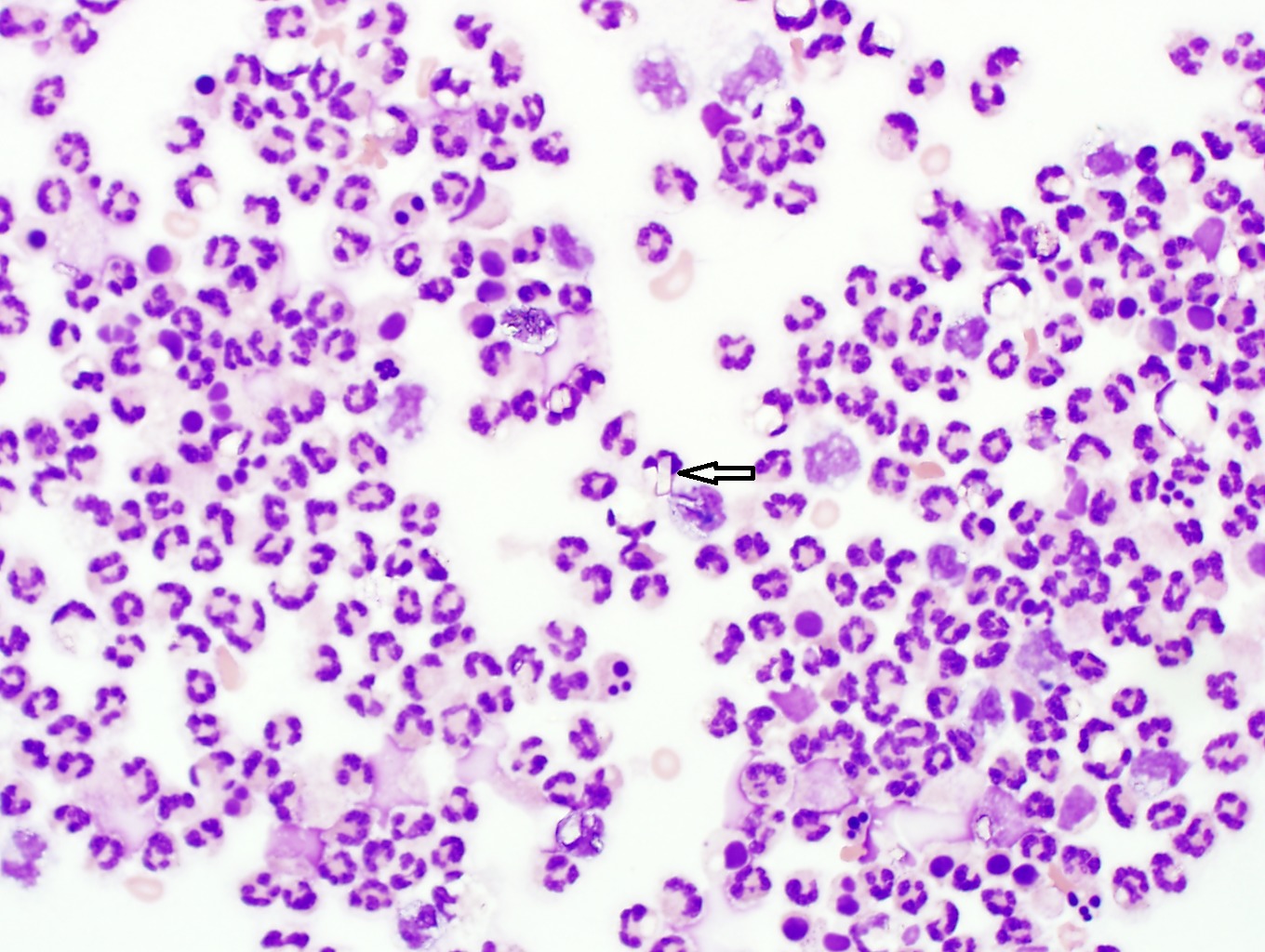
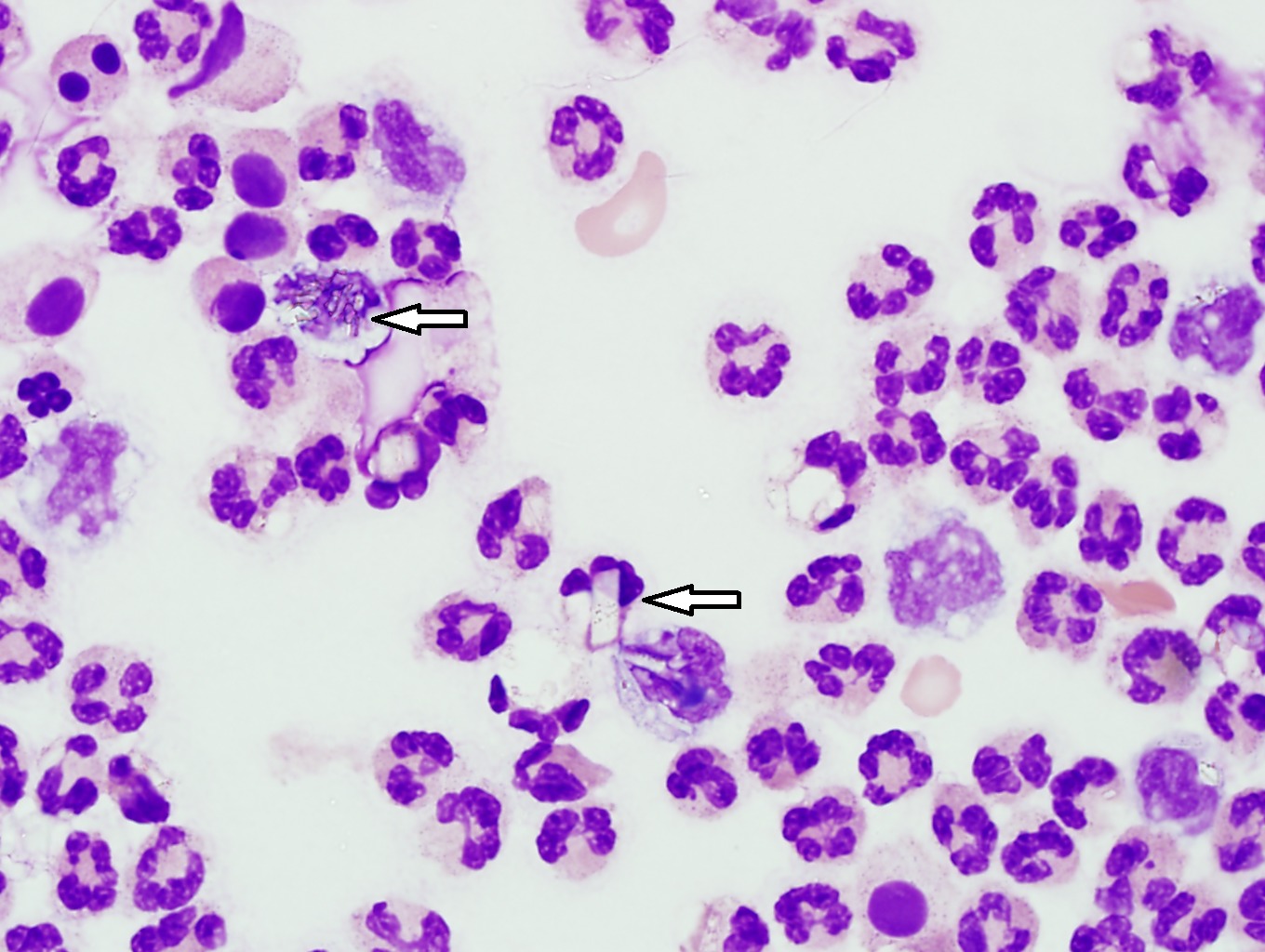
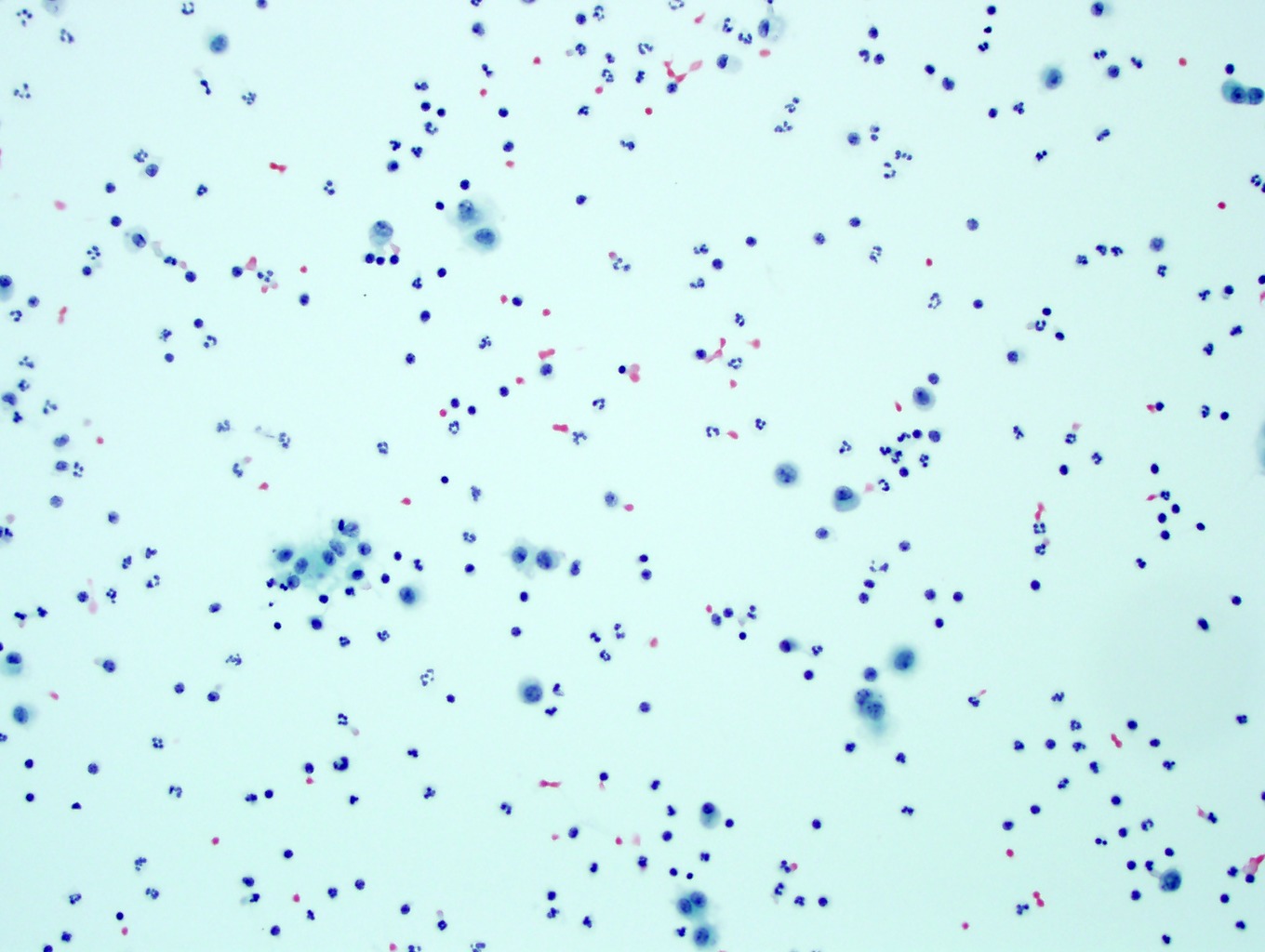
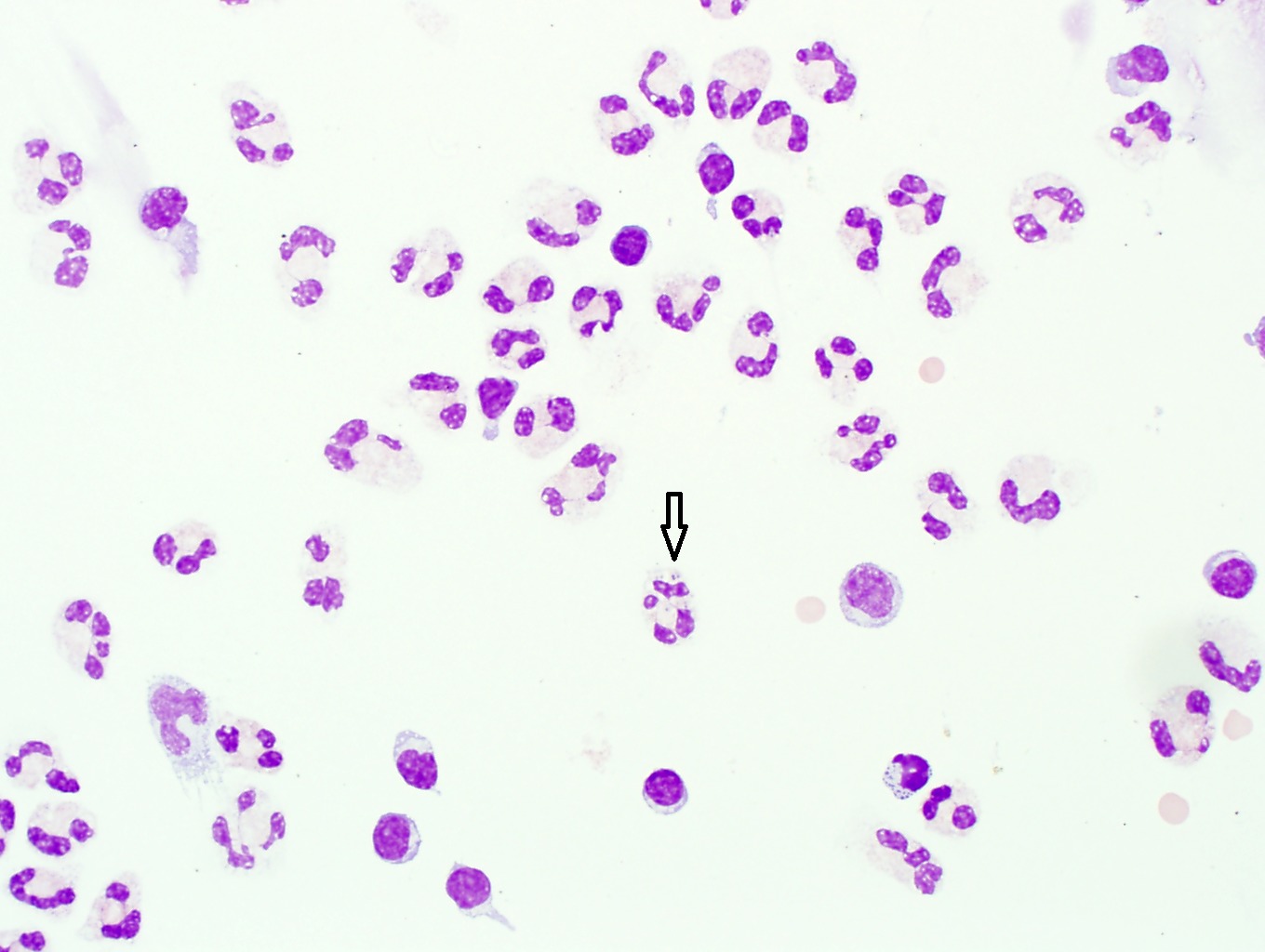
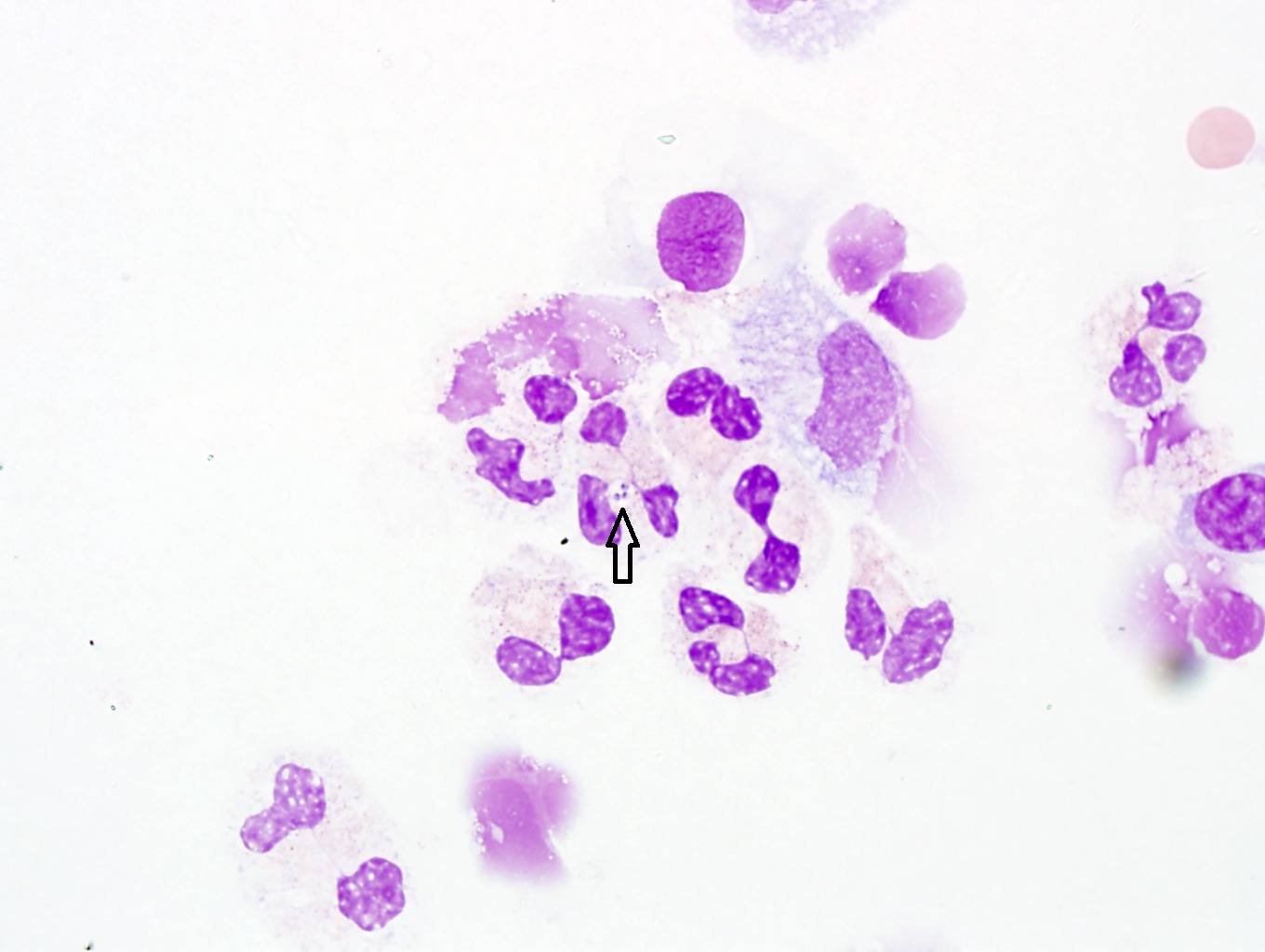
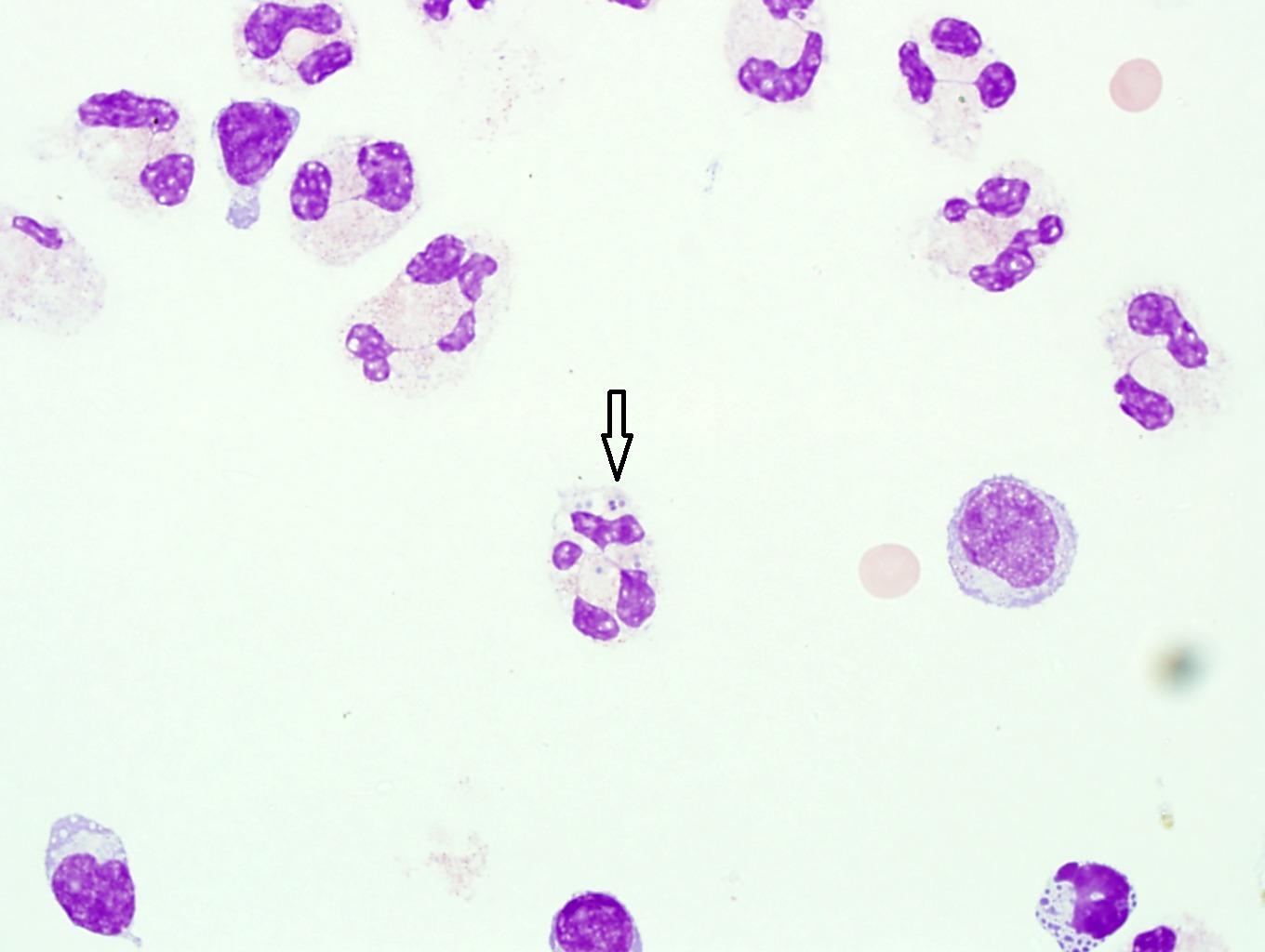
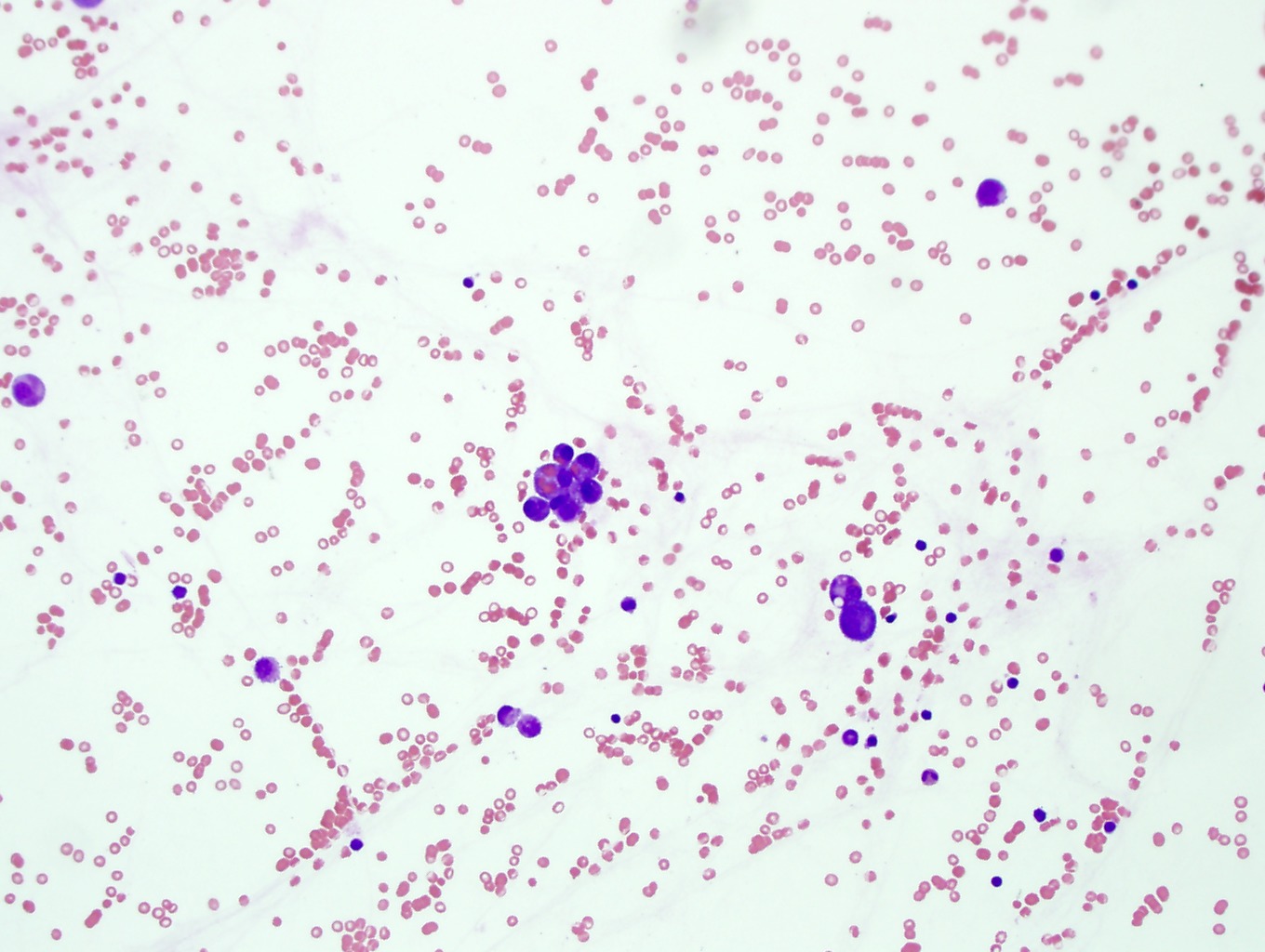
12. CSF with neutrophilia and organisms. When neutrophils are present in the CSF you must very carefully examine the cytoplasm of the cells for the presence of ingested organisms. Rare organisms are seen within a few of the neutrophils. You likely will have to look on 50X or 100X to find the organisms. See the arrows in Images 41, 42, and 43. Image 1-40, Image 1-41, Image 1-42, Image 1-43
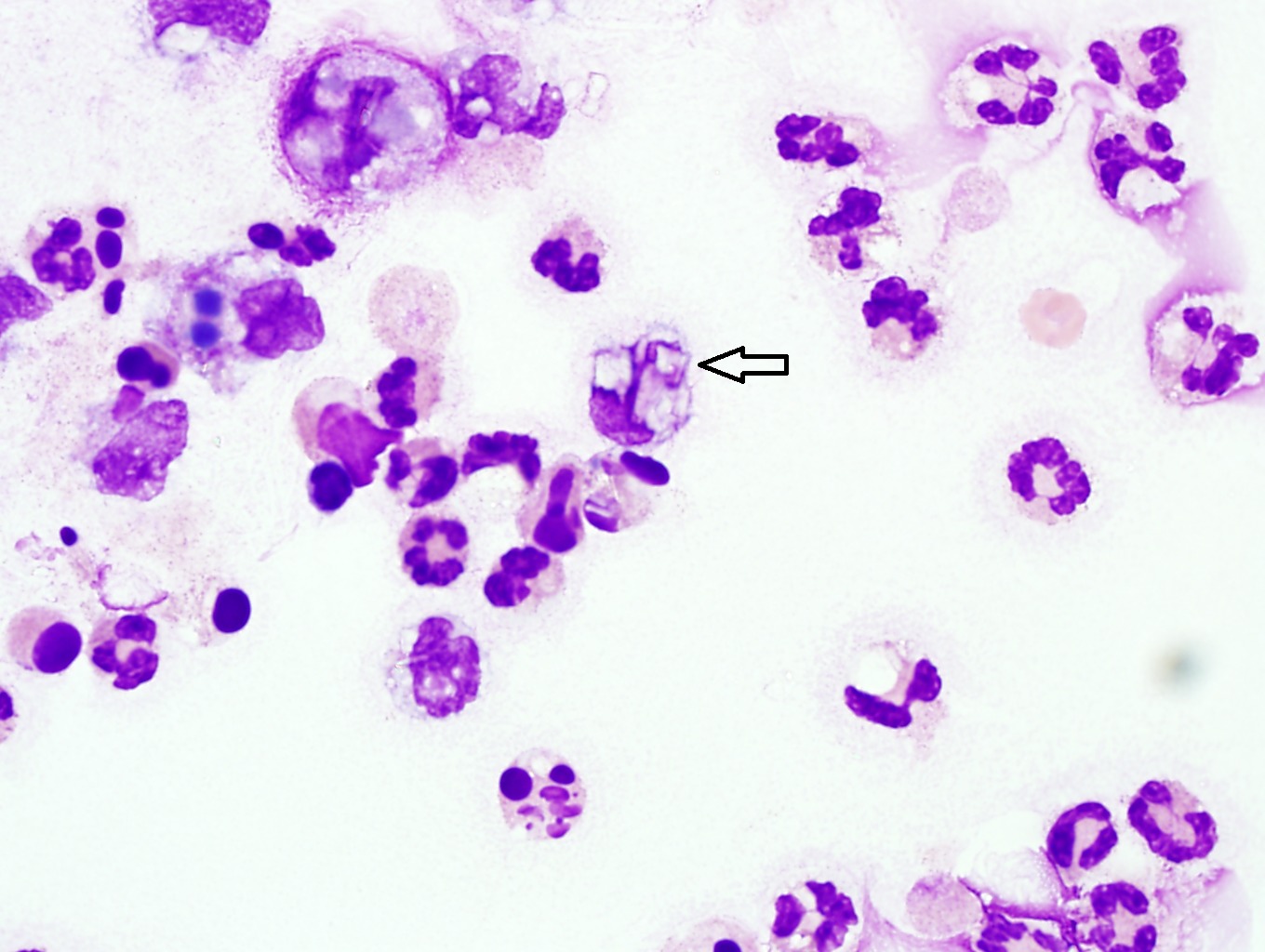
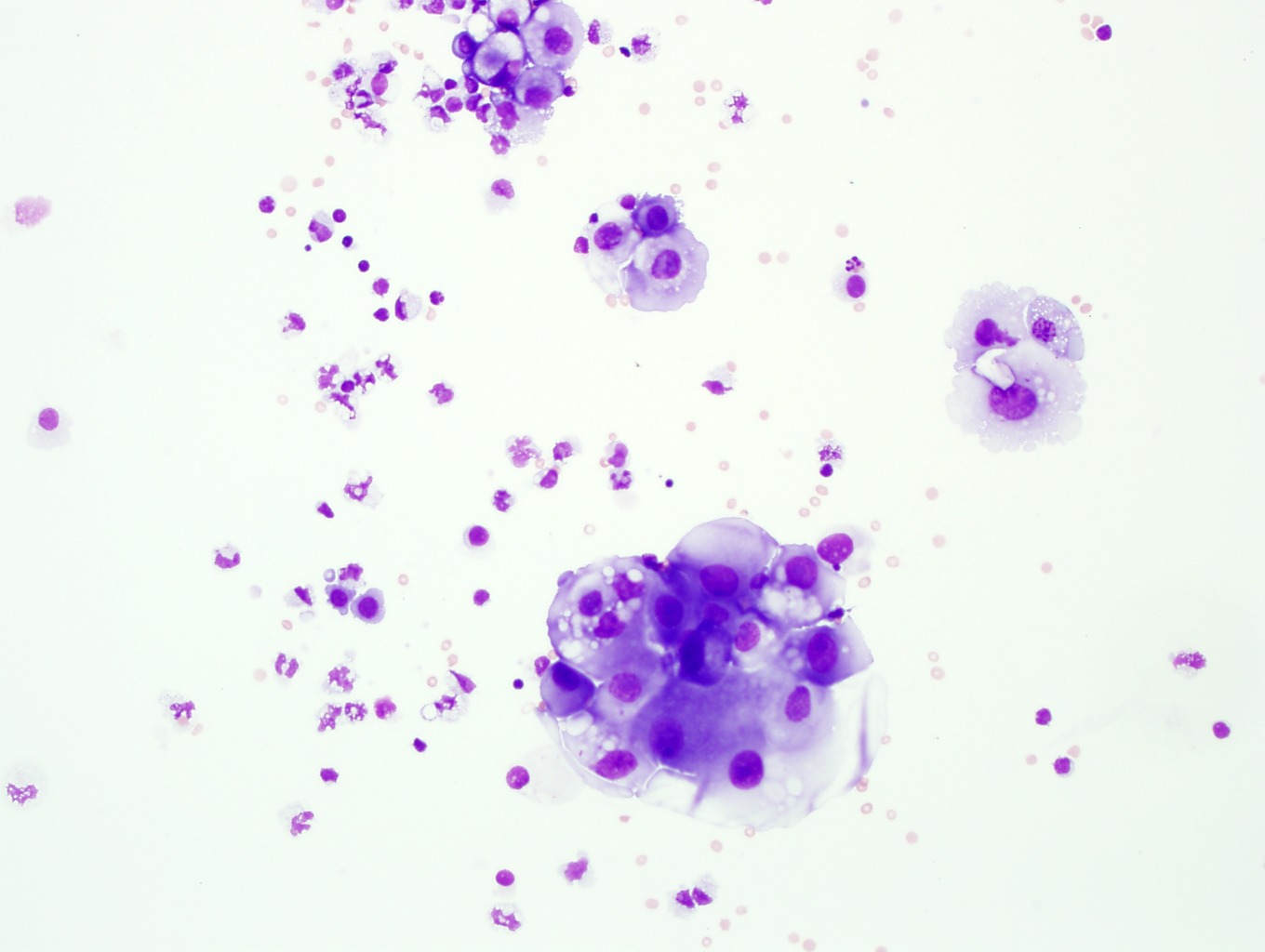
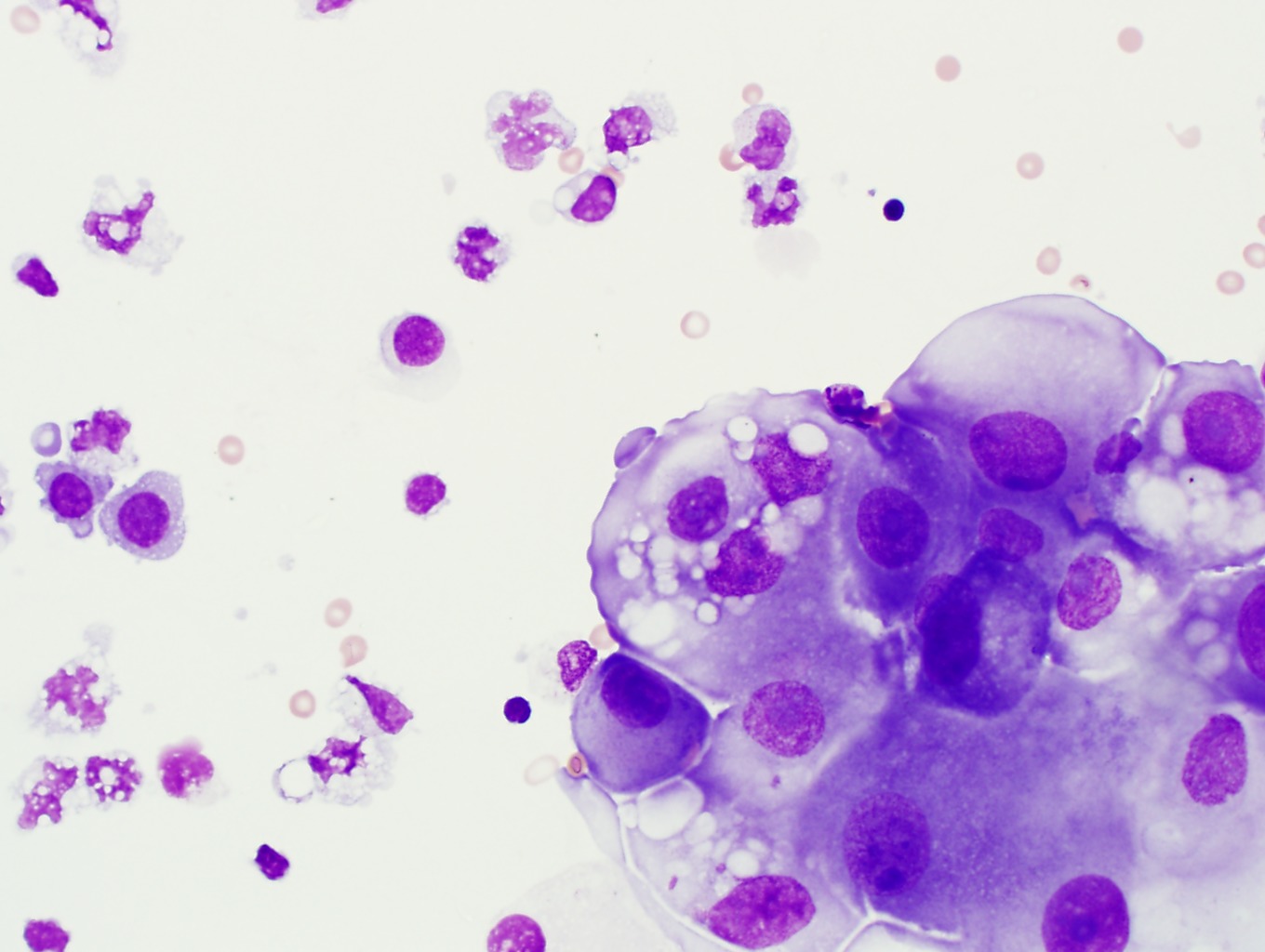
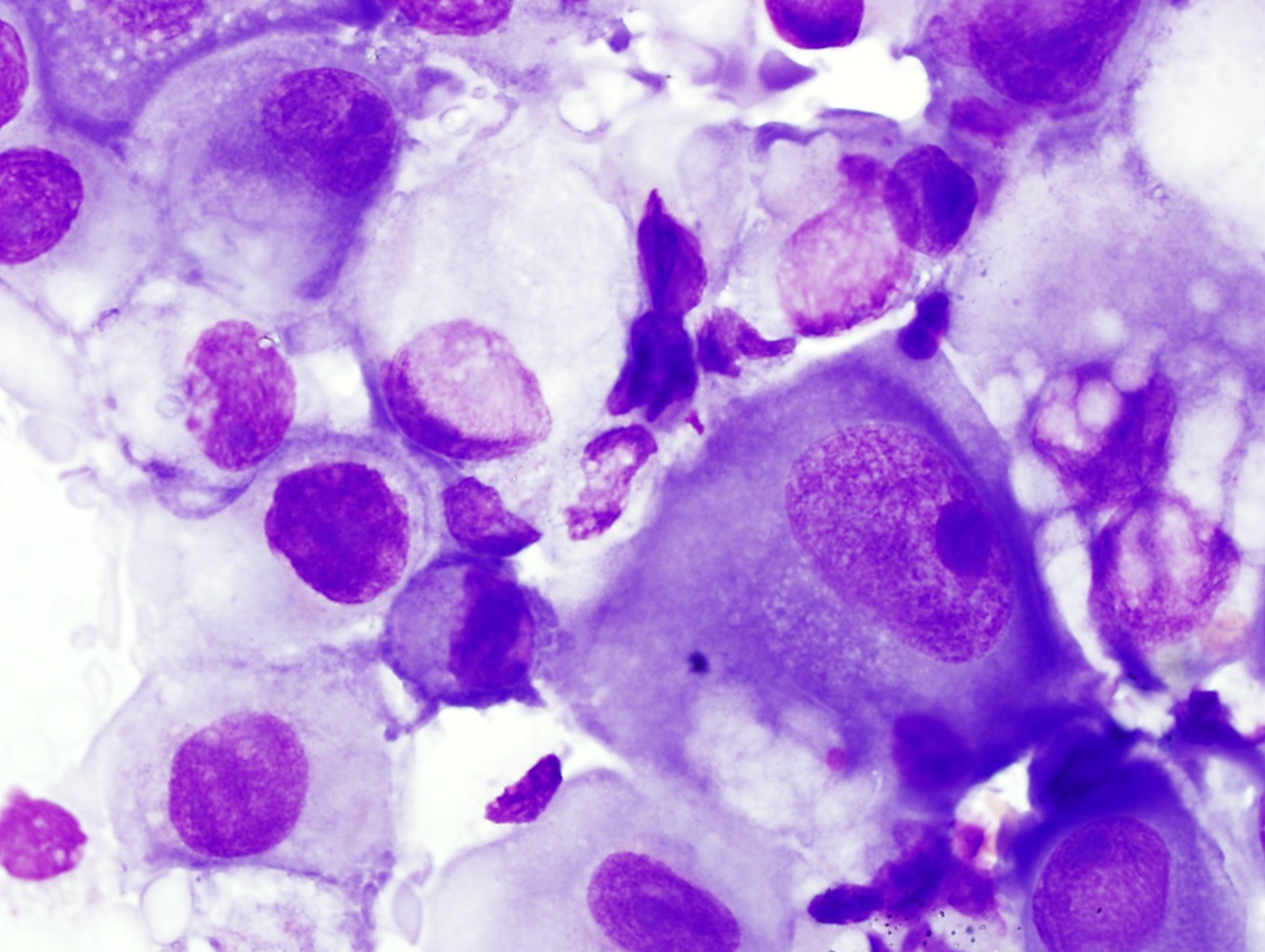
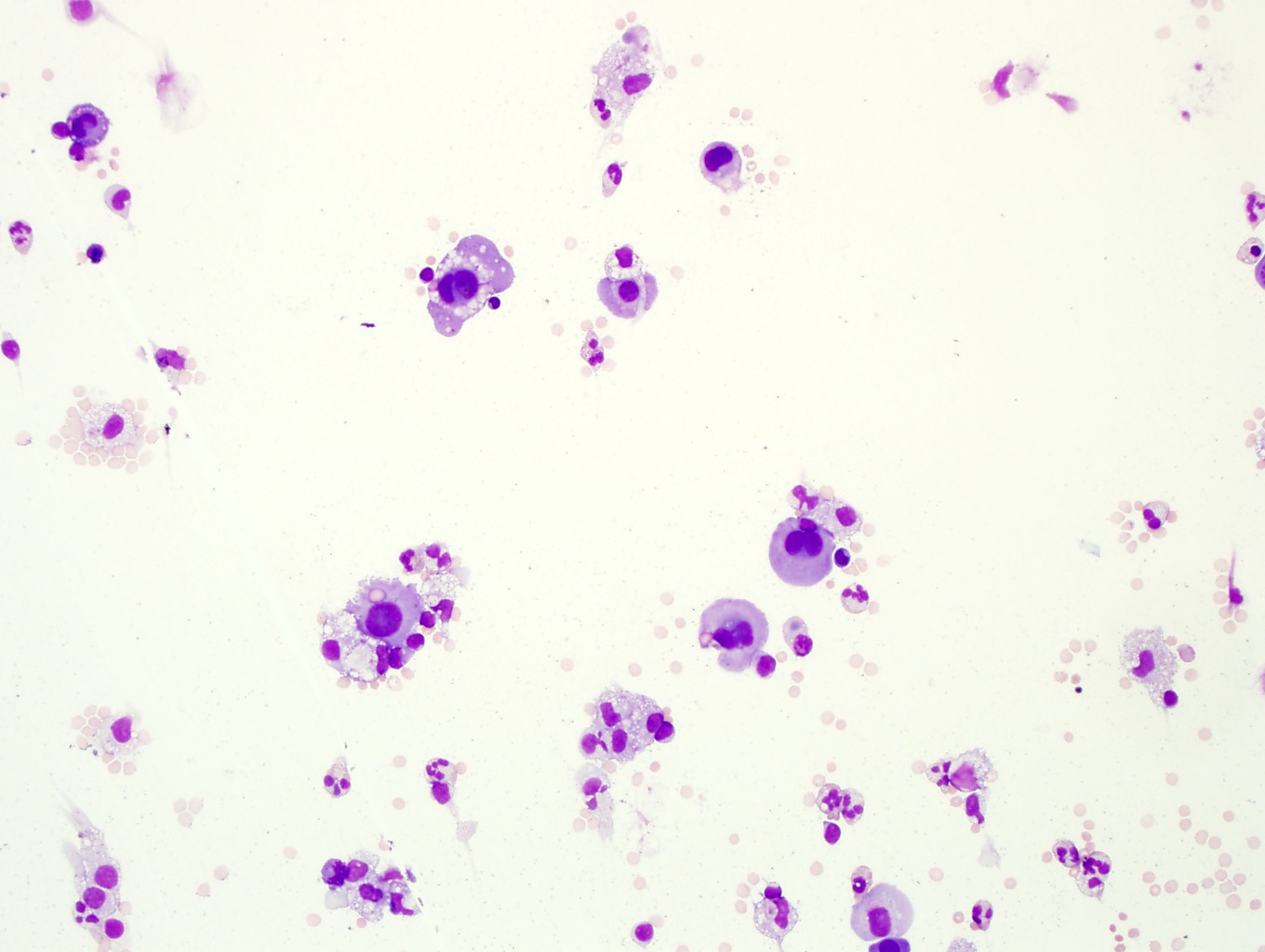
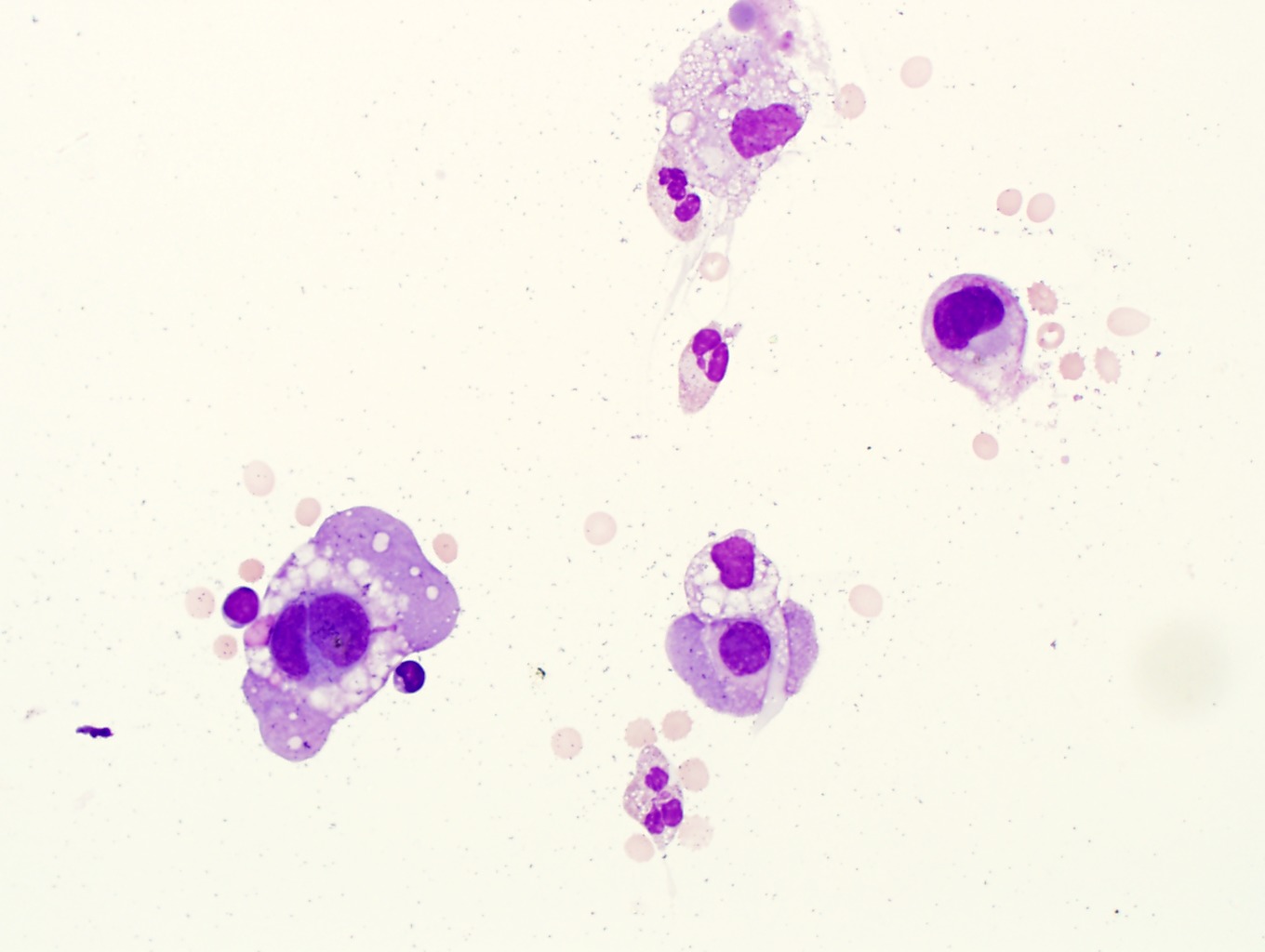
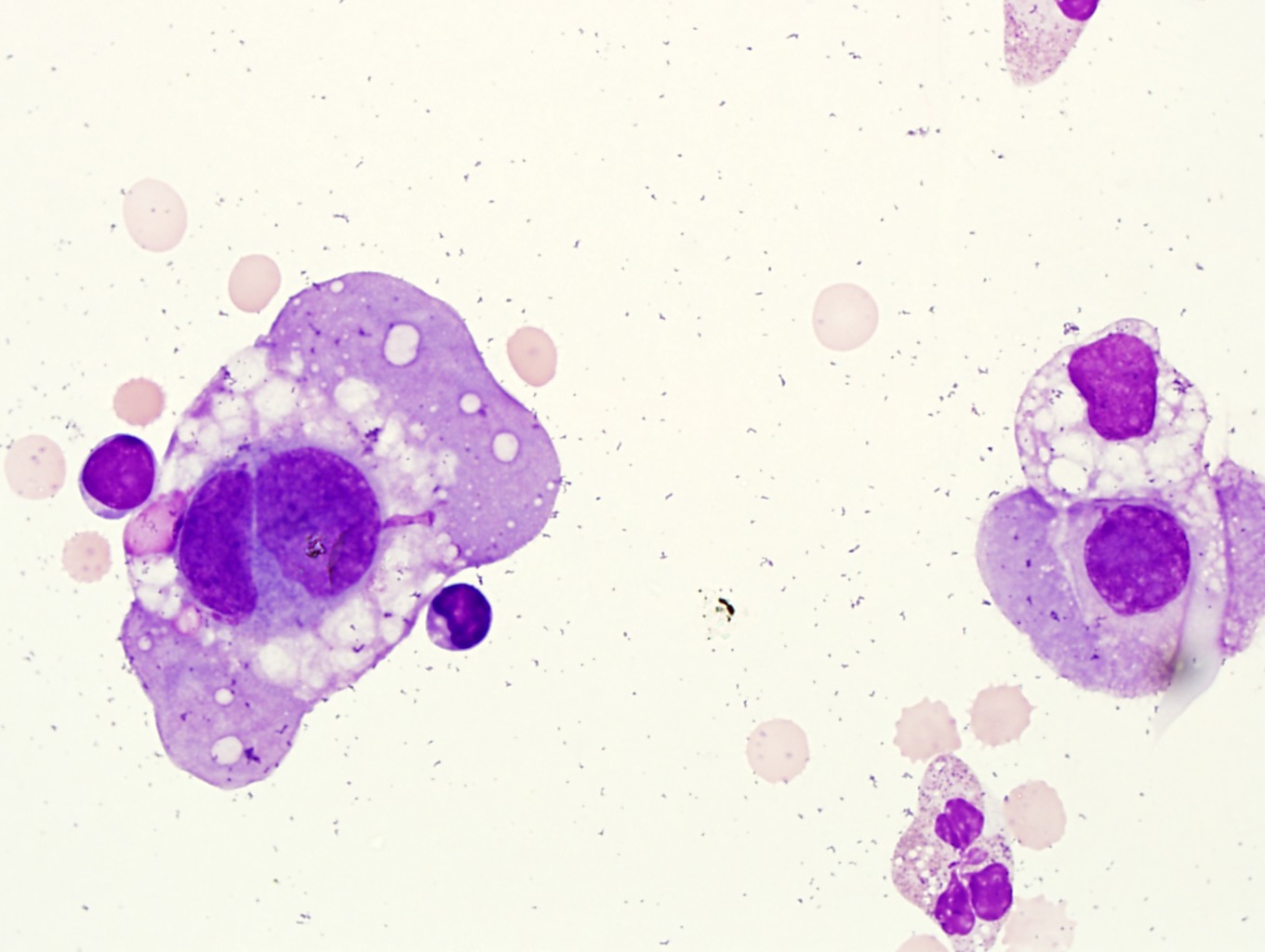
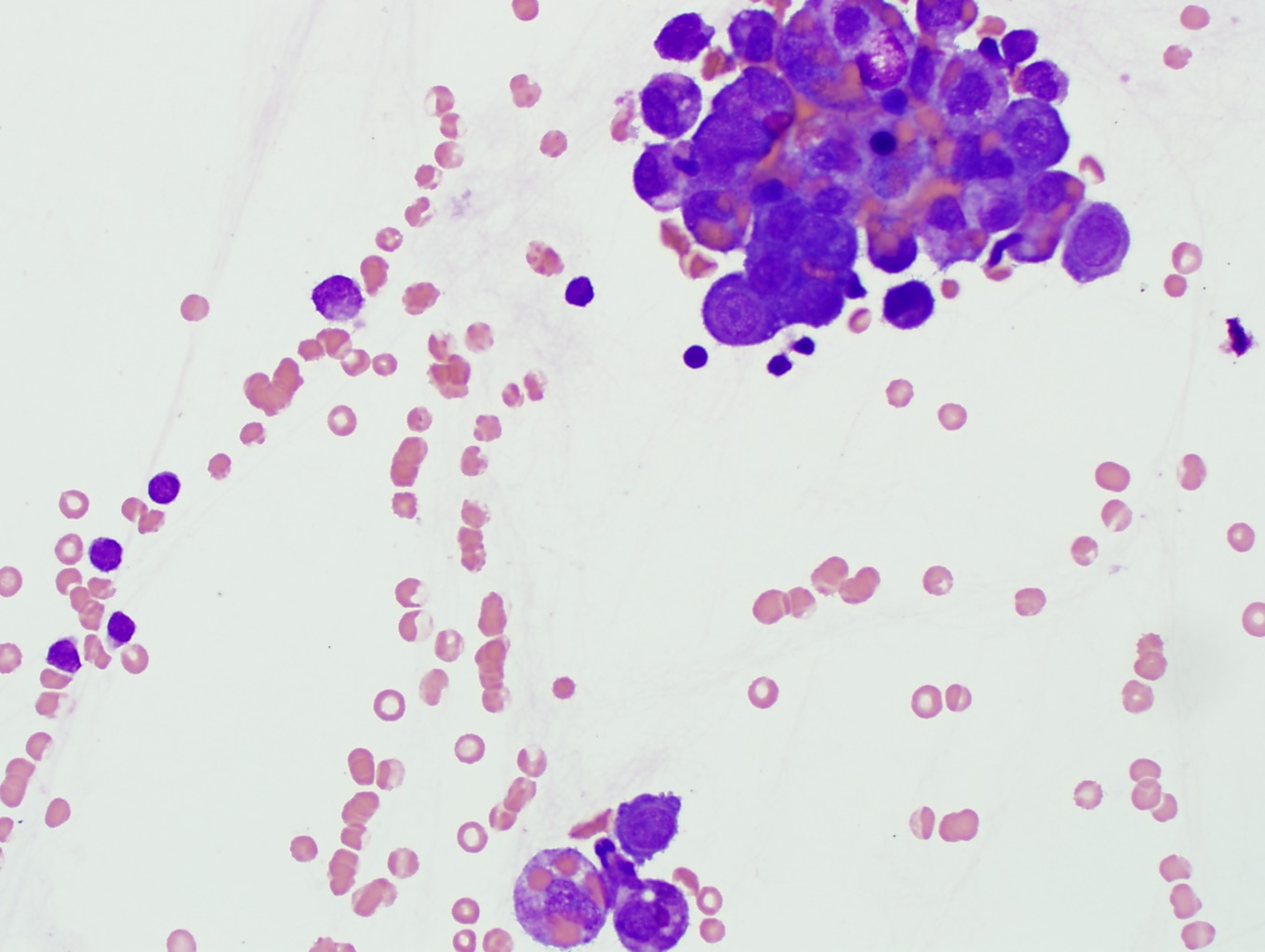
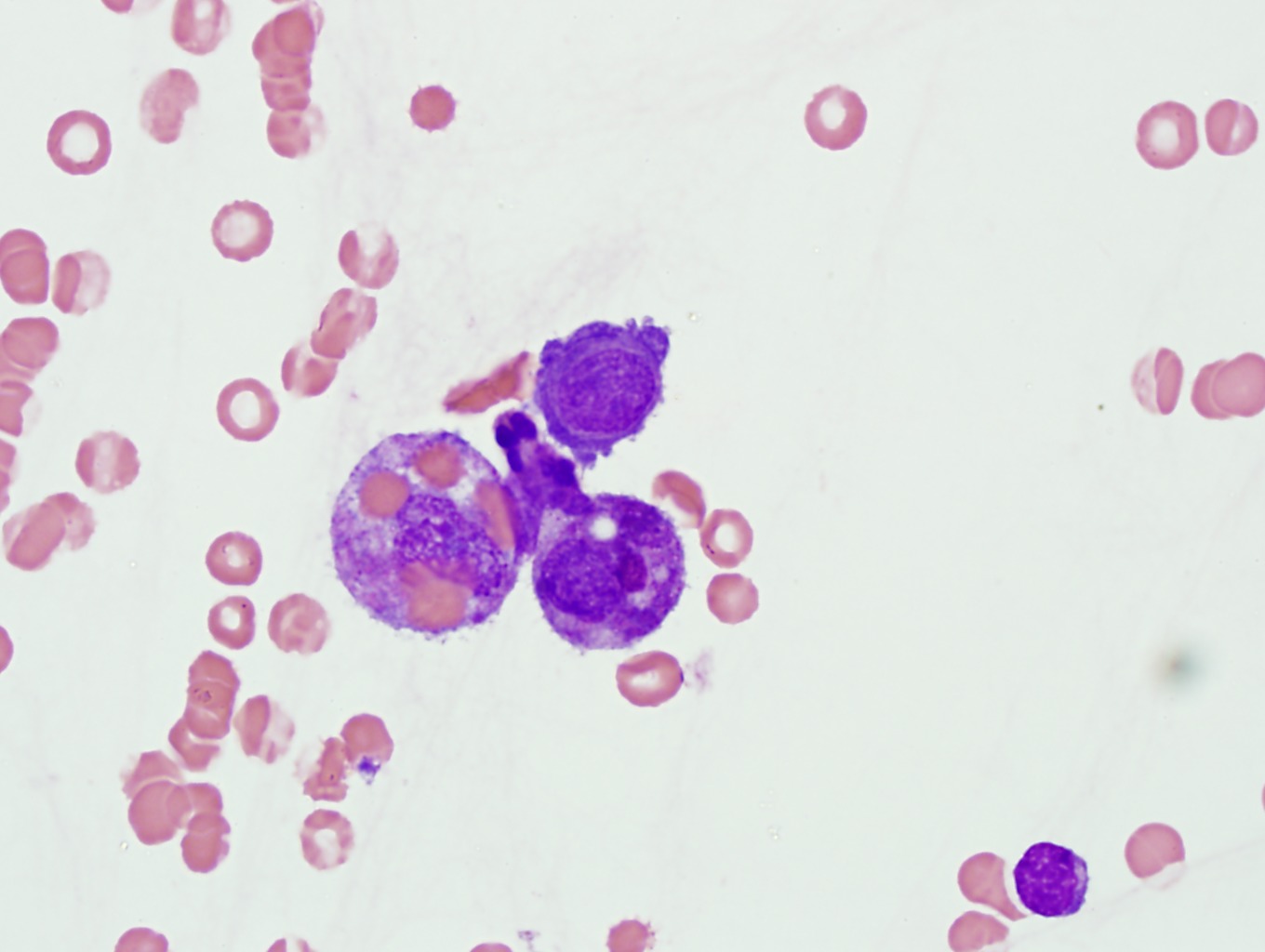
13. CSF with metastatic neuroendocrine carcinoma and hemophagocytosis. Note the clumping of the tumor cells and the nuclear molding typical of neuroendocrine cell carcinoma. There is also prominent hemophagocytosis. Image1-44, Image 1-45, Image 1-46, Image 1-47
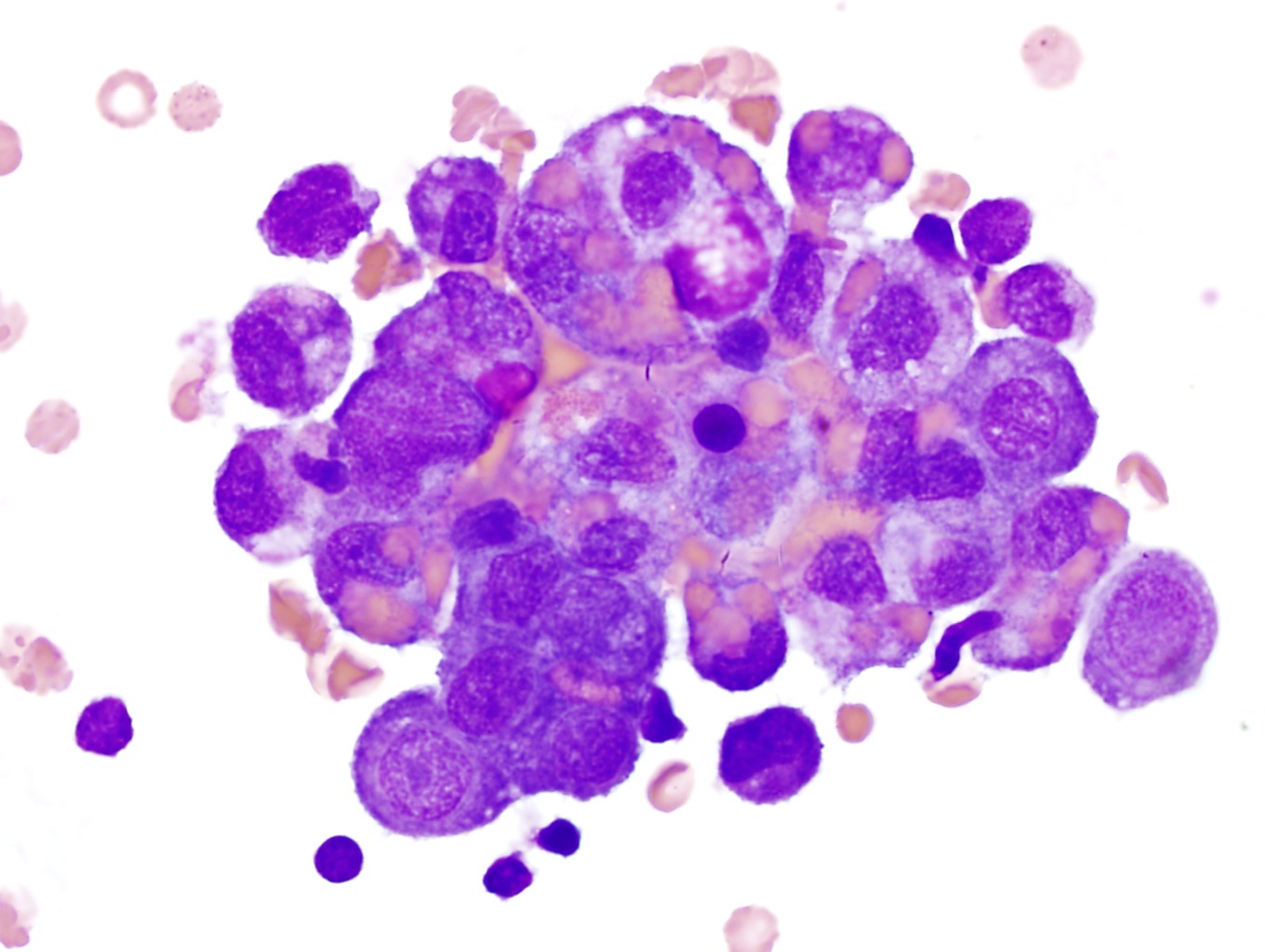
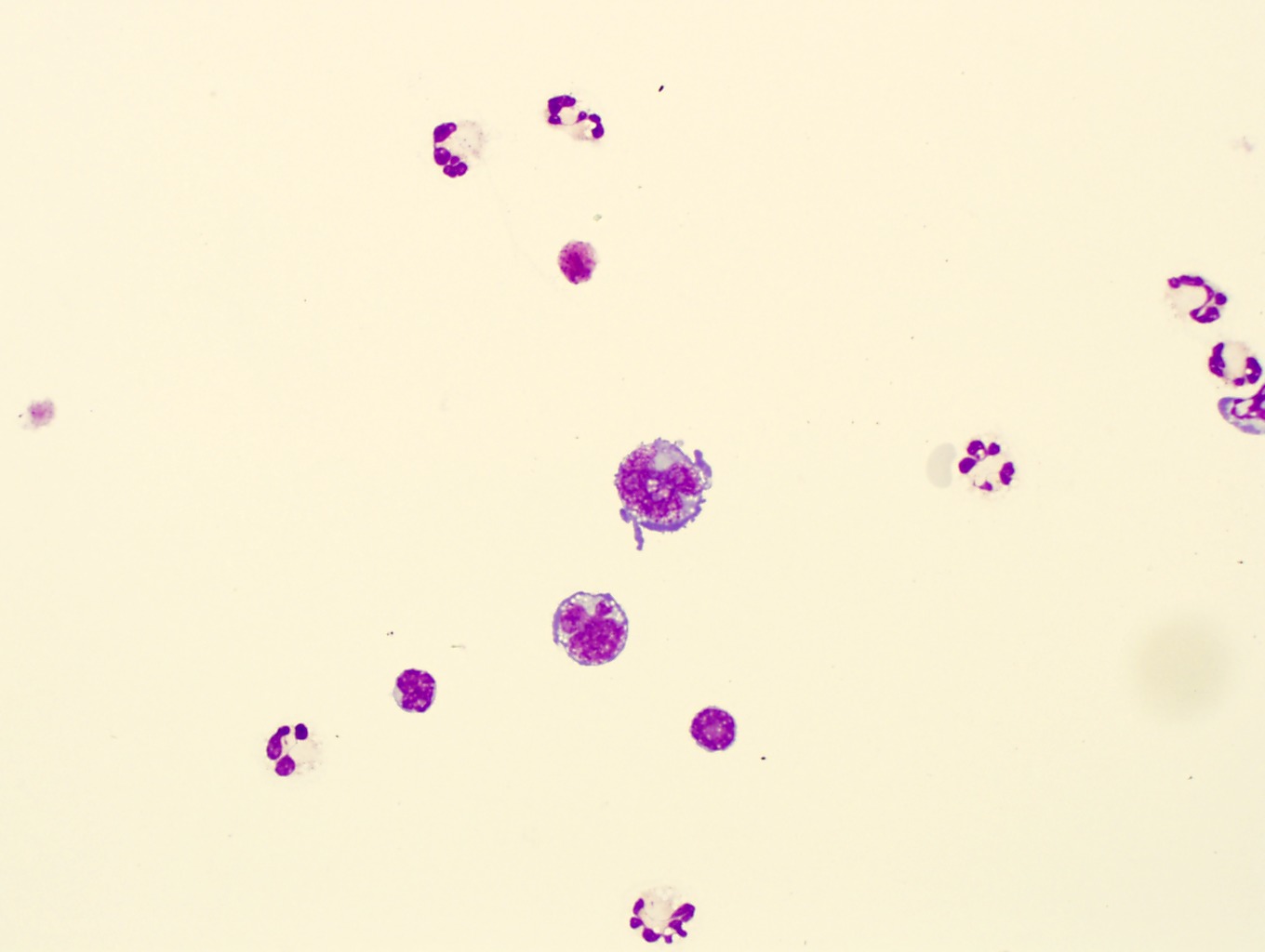
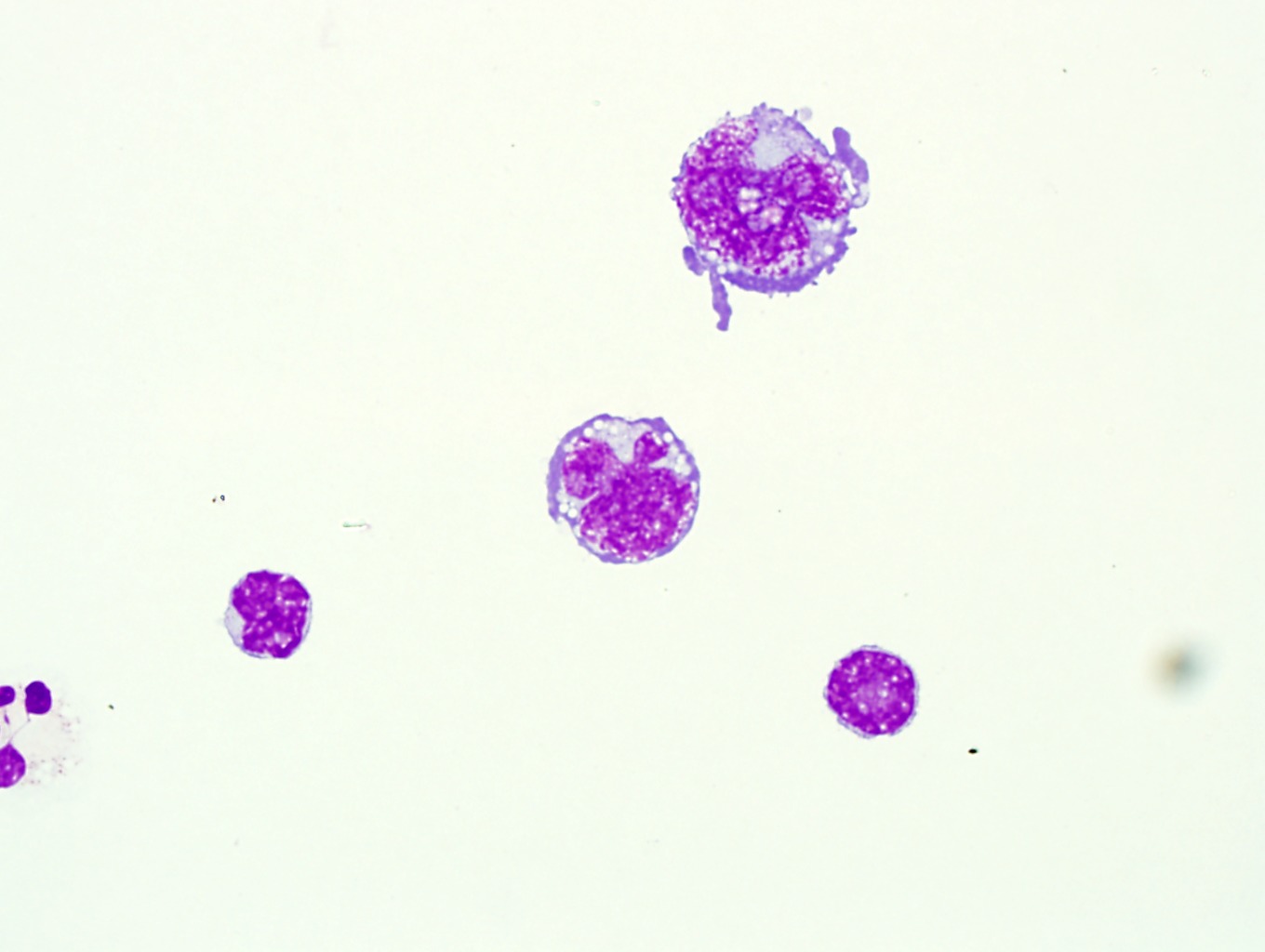
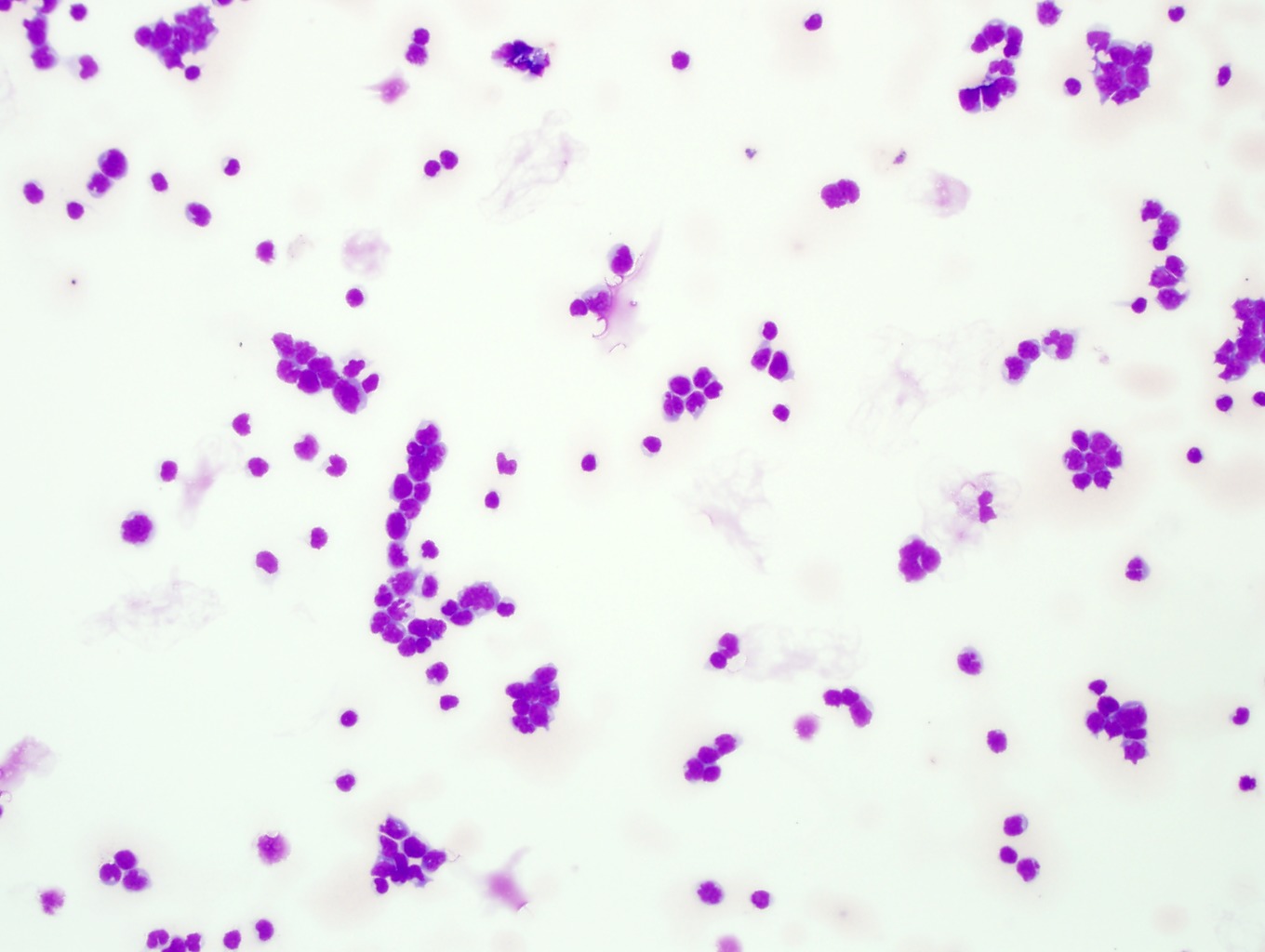
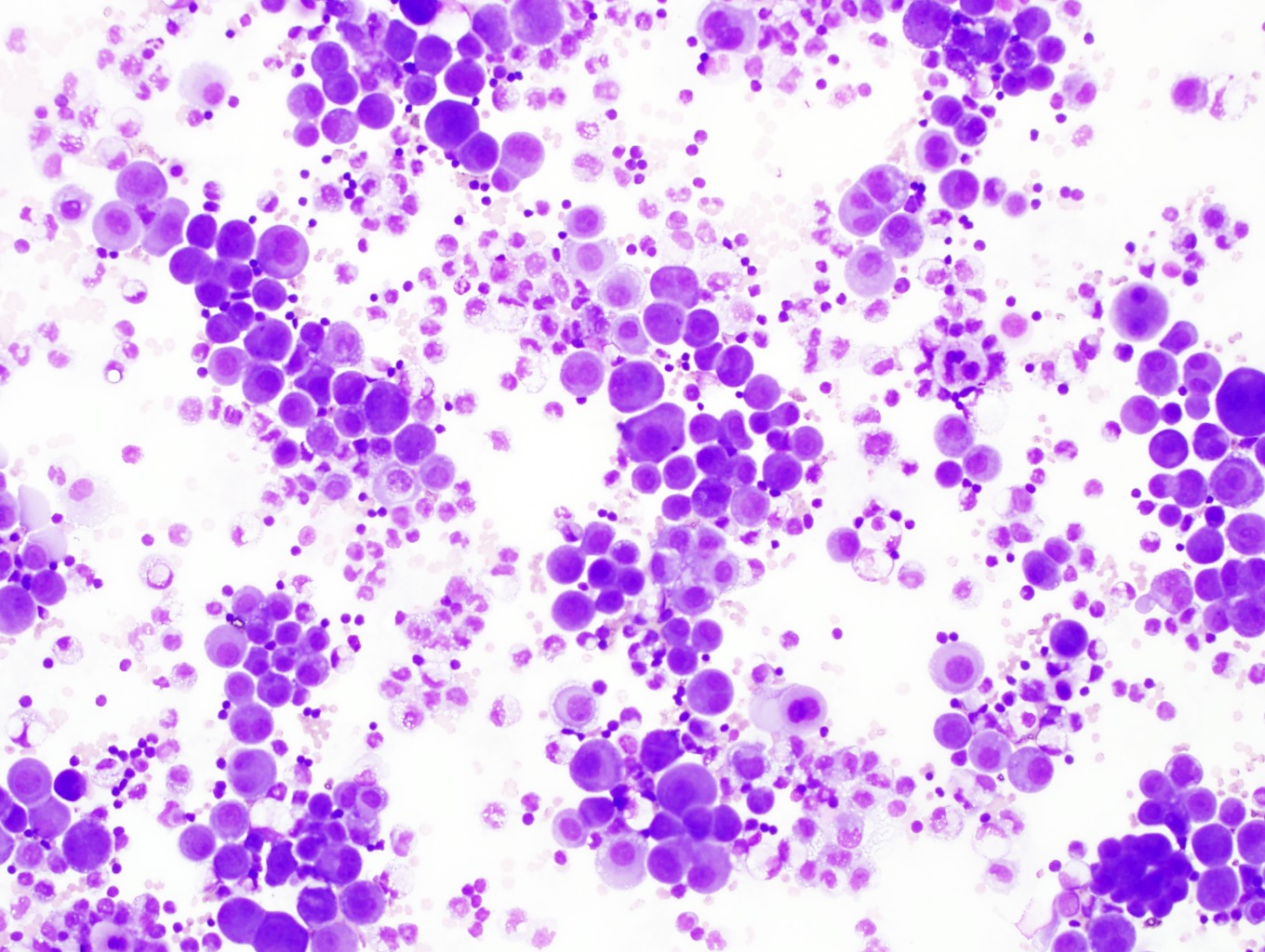
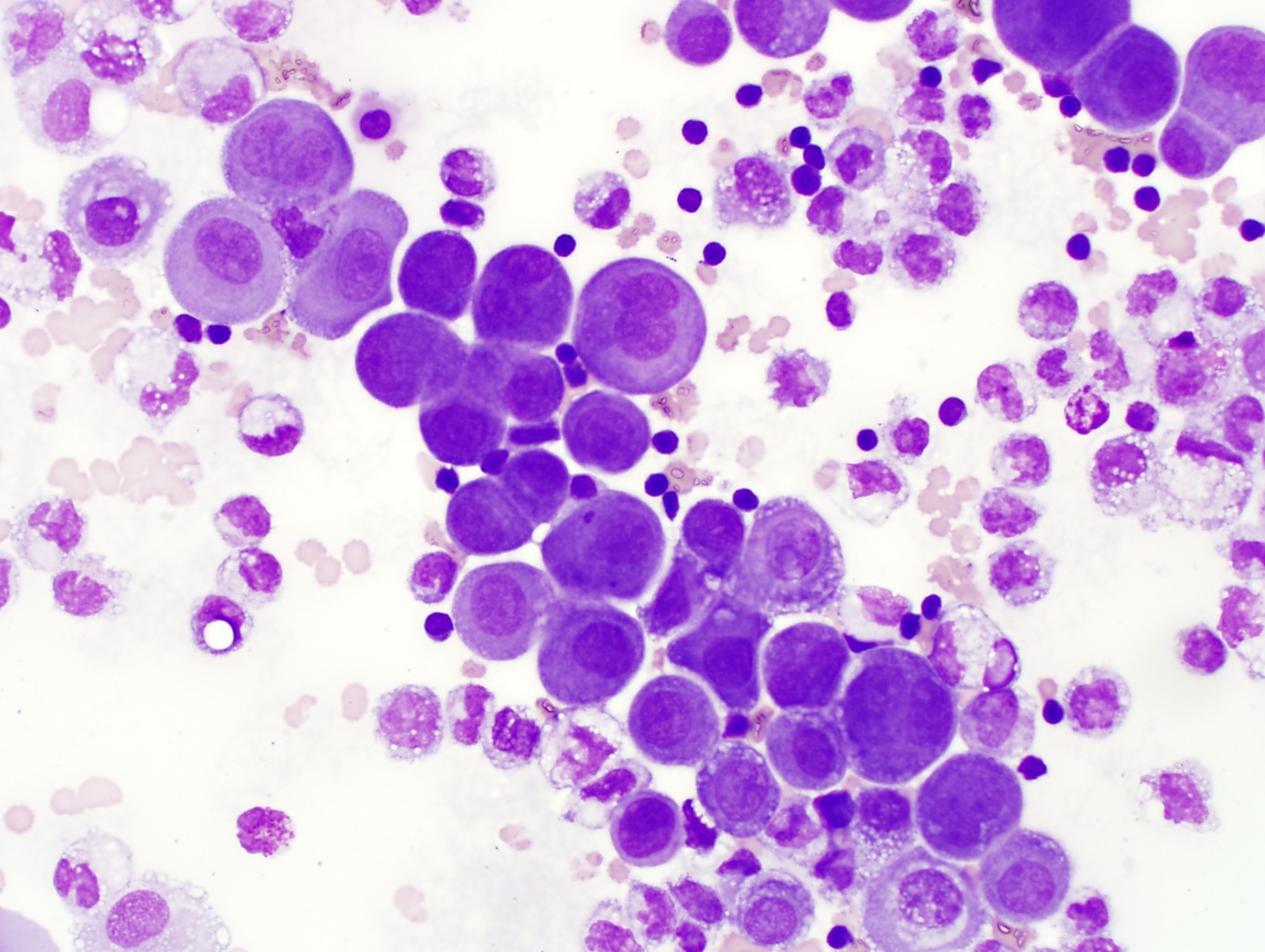
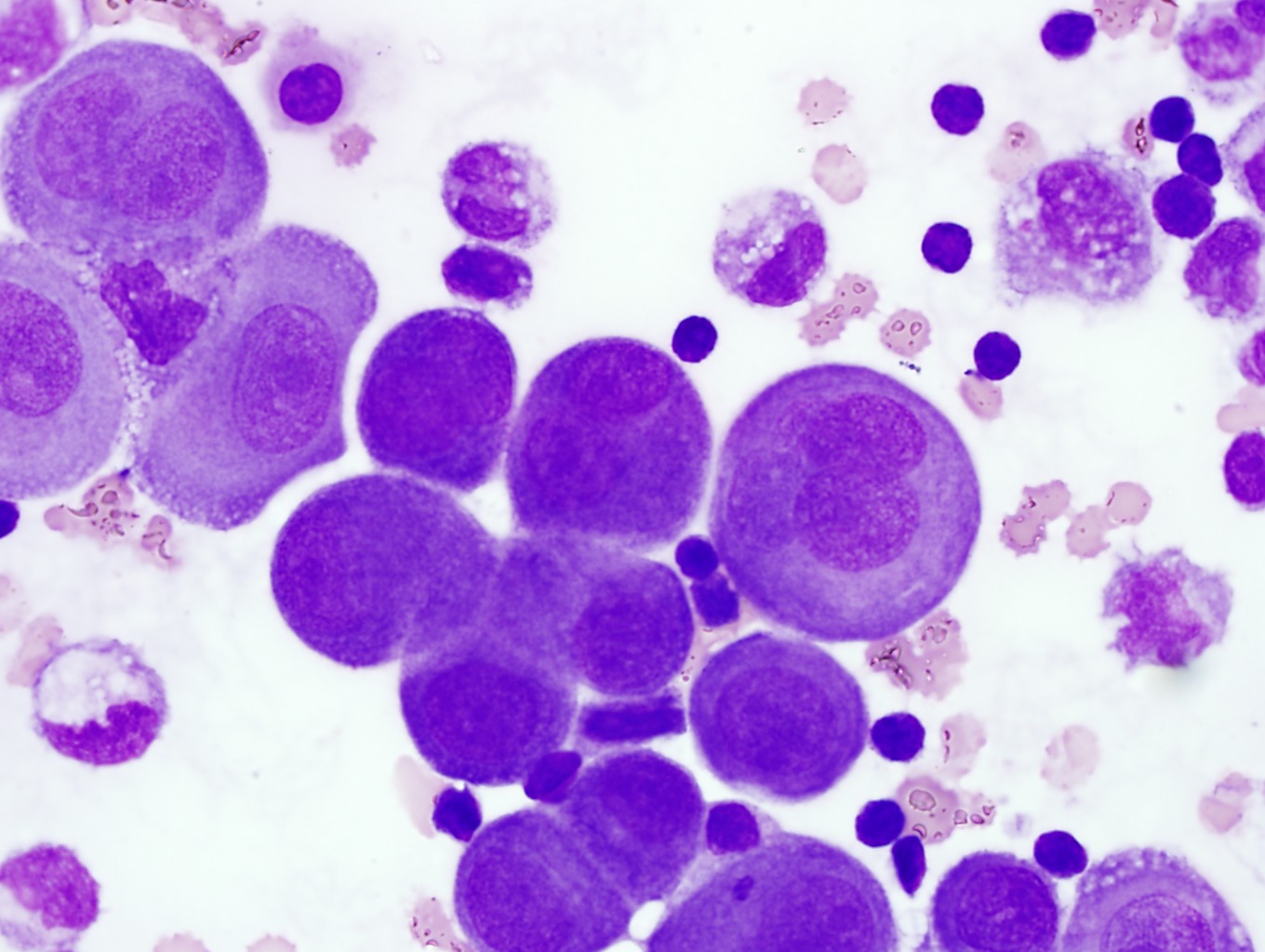
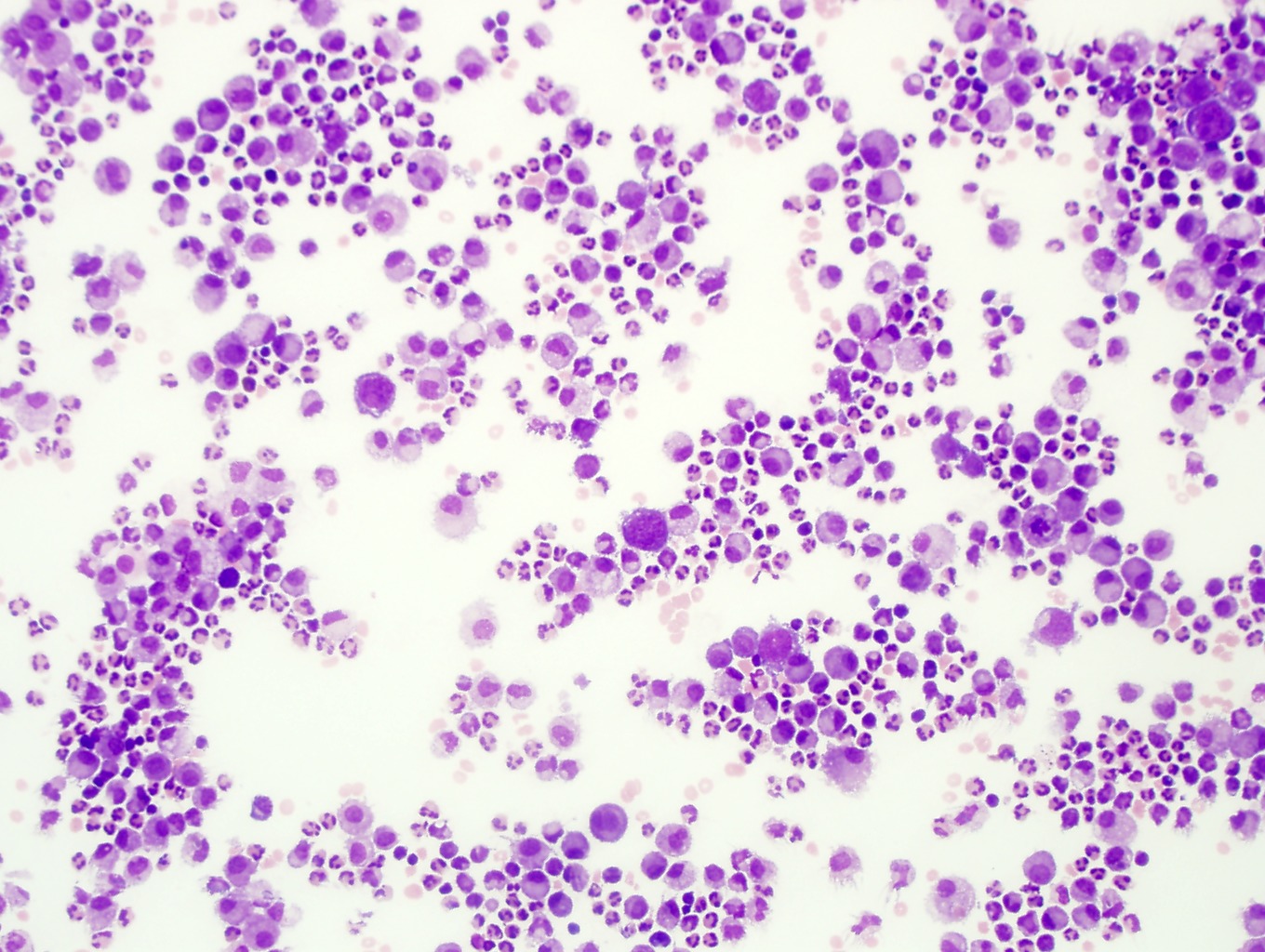
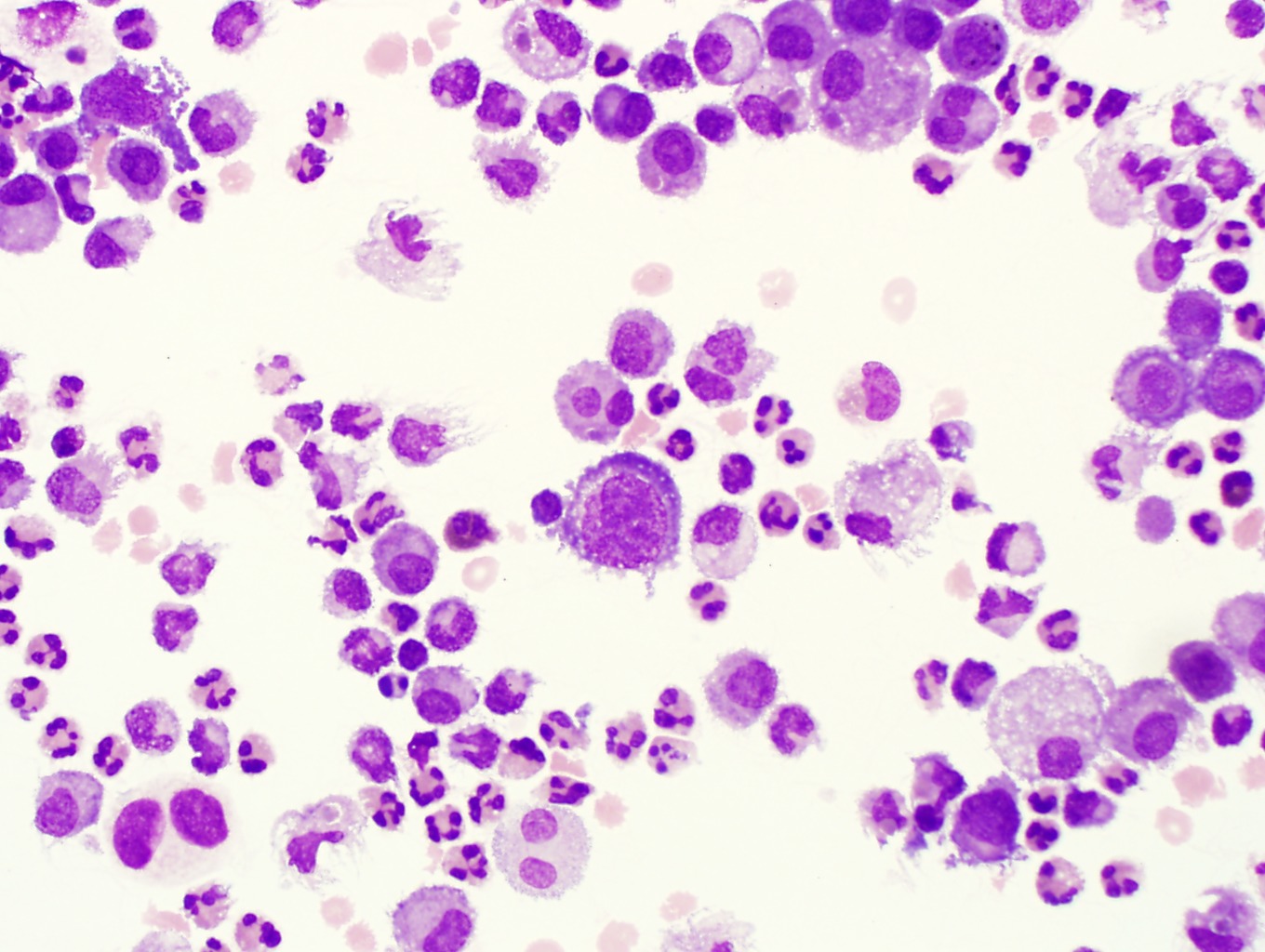
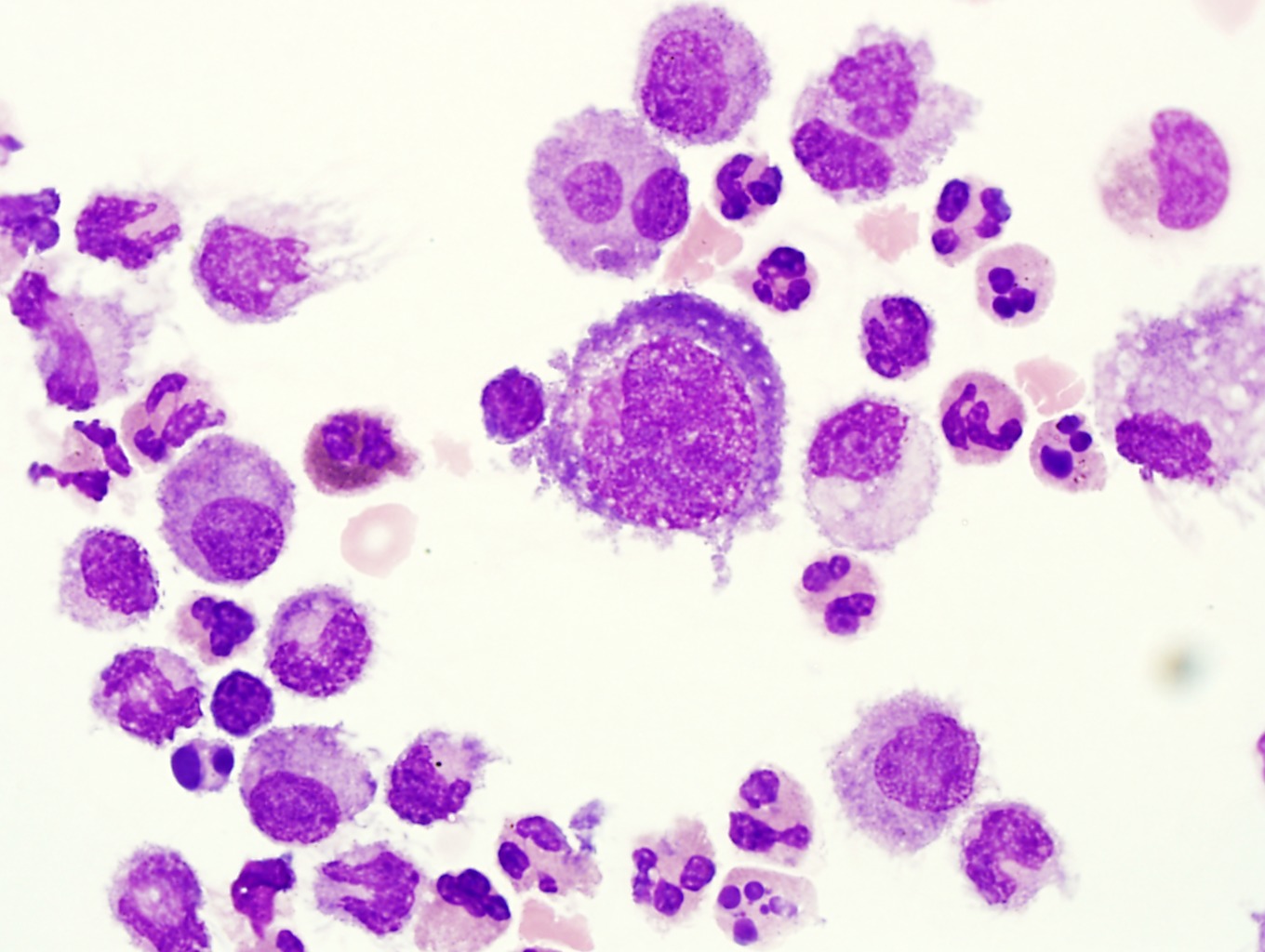
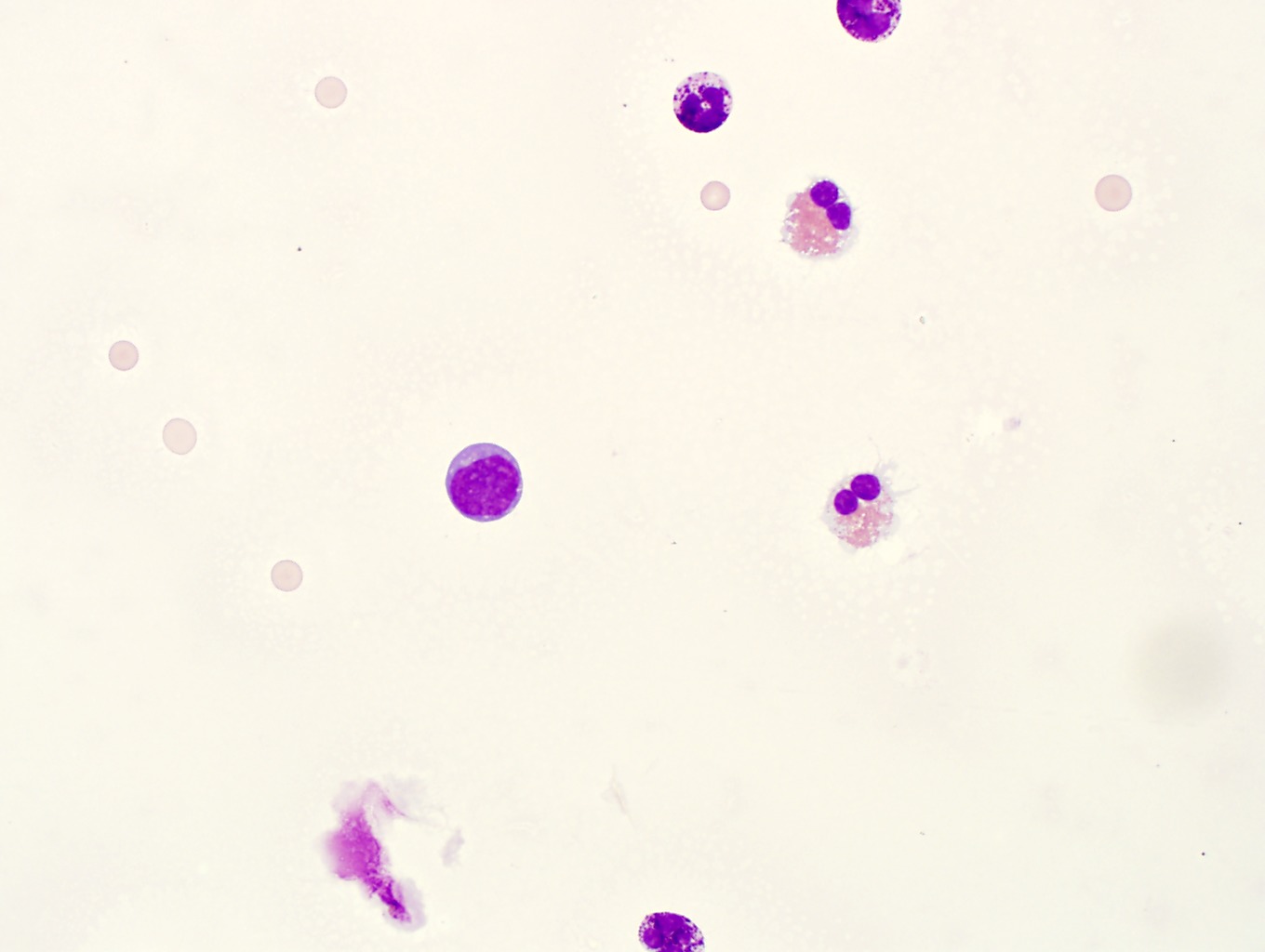
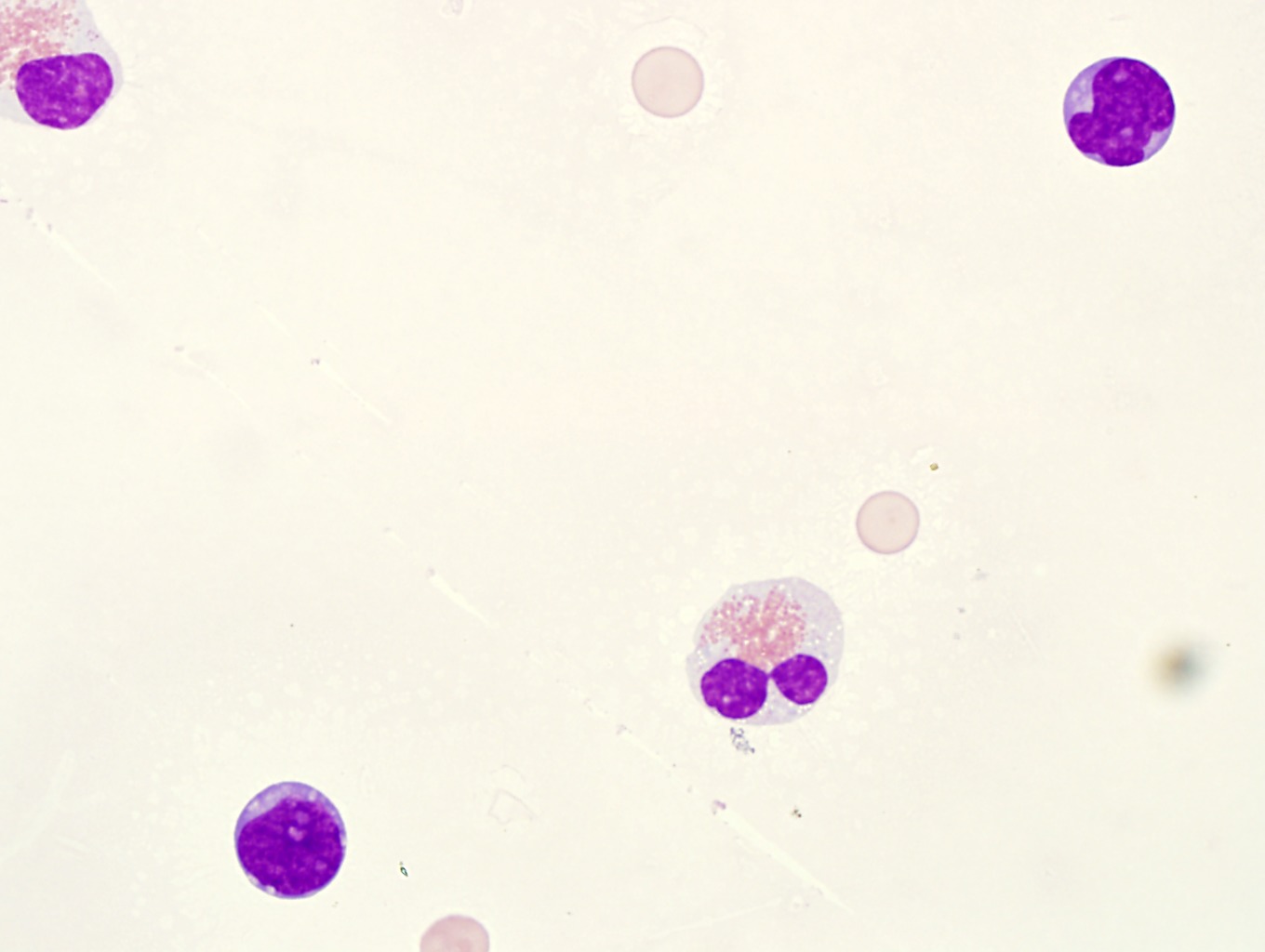
14. CSF with involvement by acute myeloid leukemia (AML). Note the fine chromatin, prominent nucleoli, and cytoplasmic granules of the atypical cells. These are myeloblasts in a patient with AML. Compare these cells to the adjacent mature lymphocytes (which are smaller with more condensed chromatin). A myeloperoxidase stain should be positive and flow cytometry would demonstrate these cells are myeloid blasts. Image 1-48, Image 1-49, Image 1-50
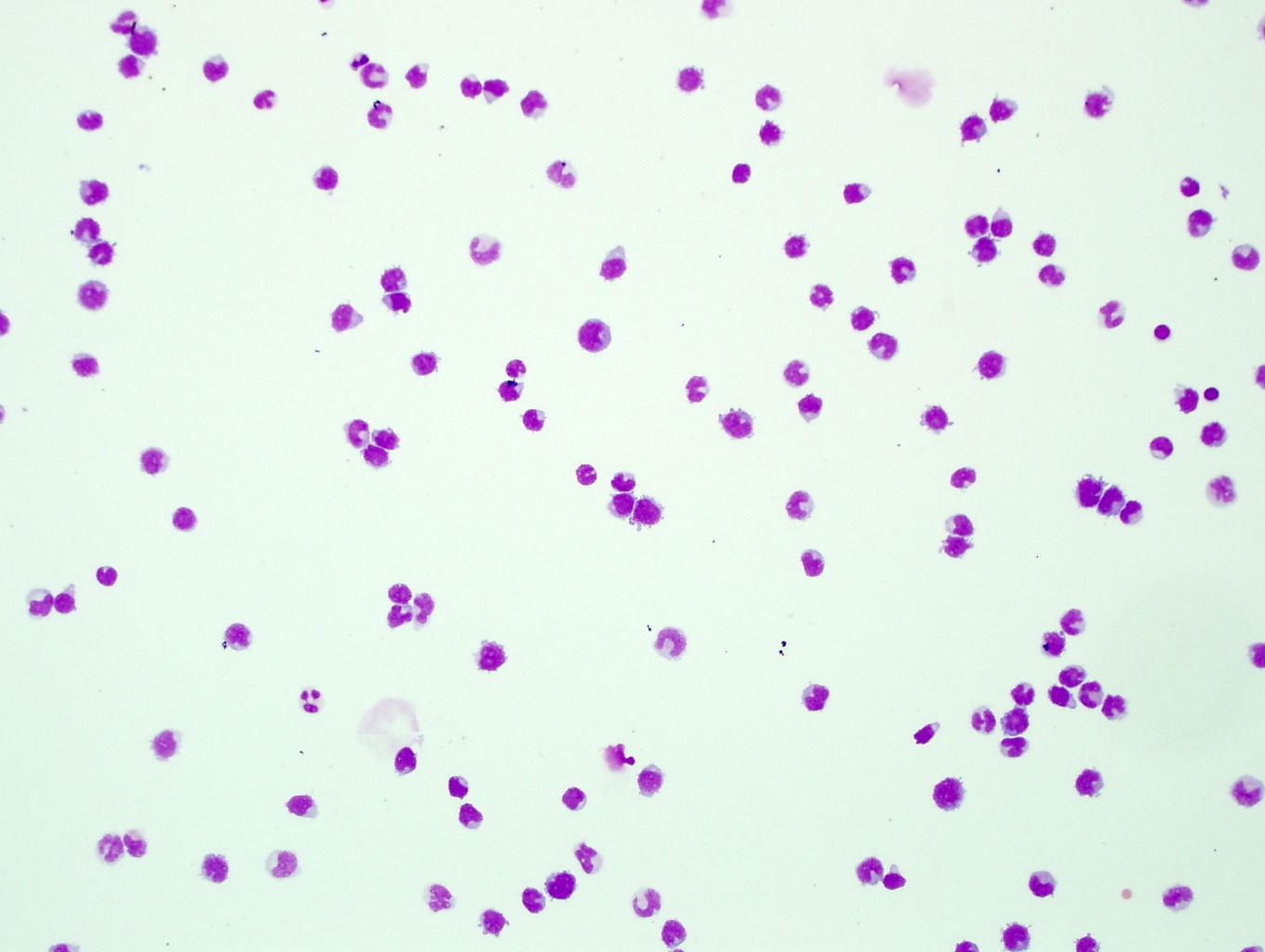
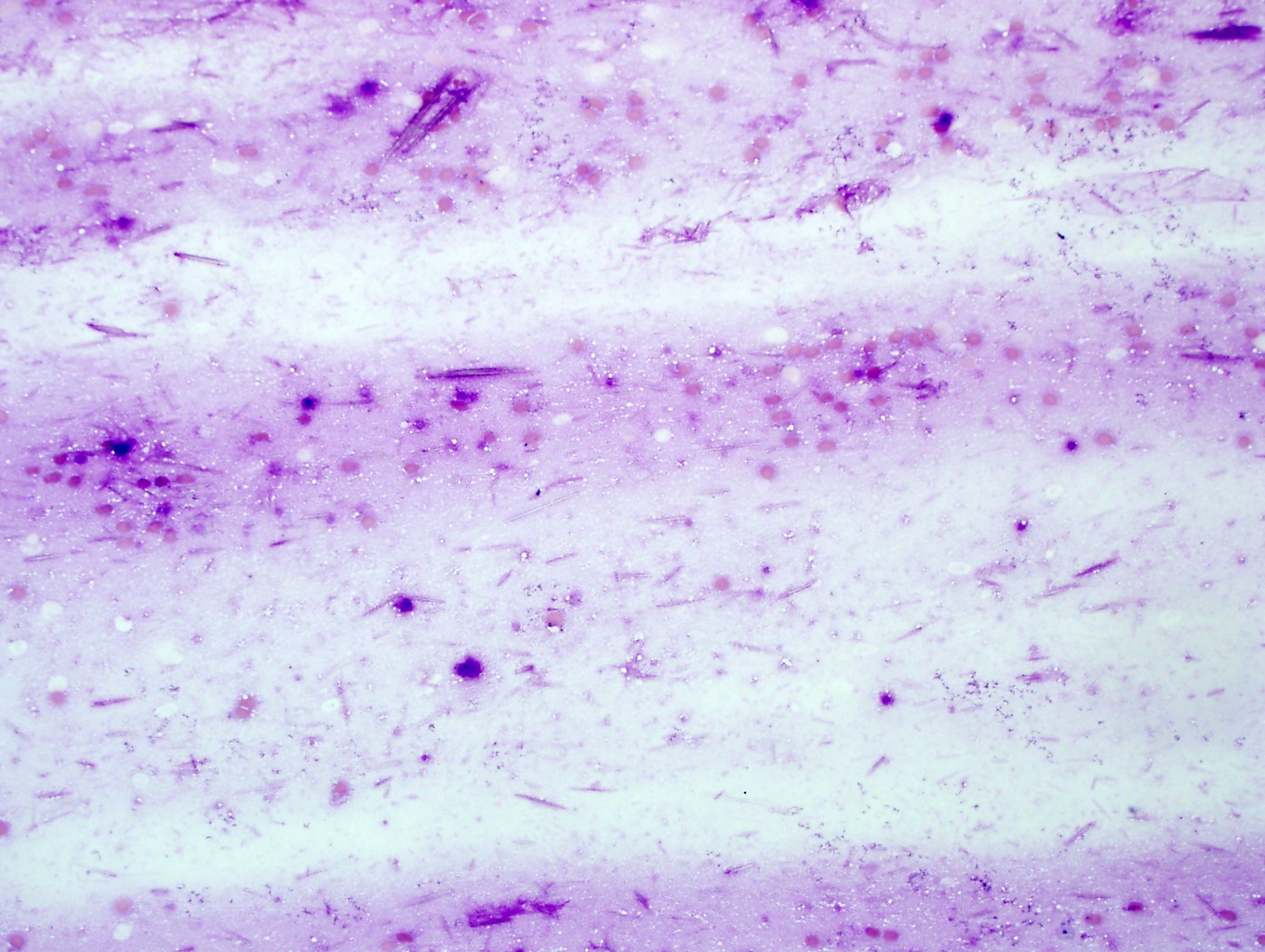
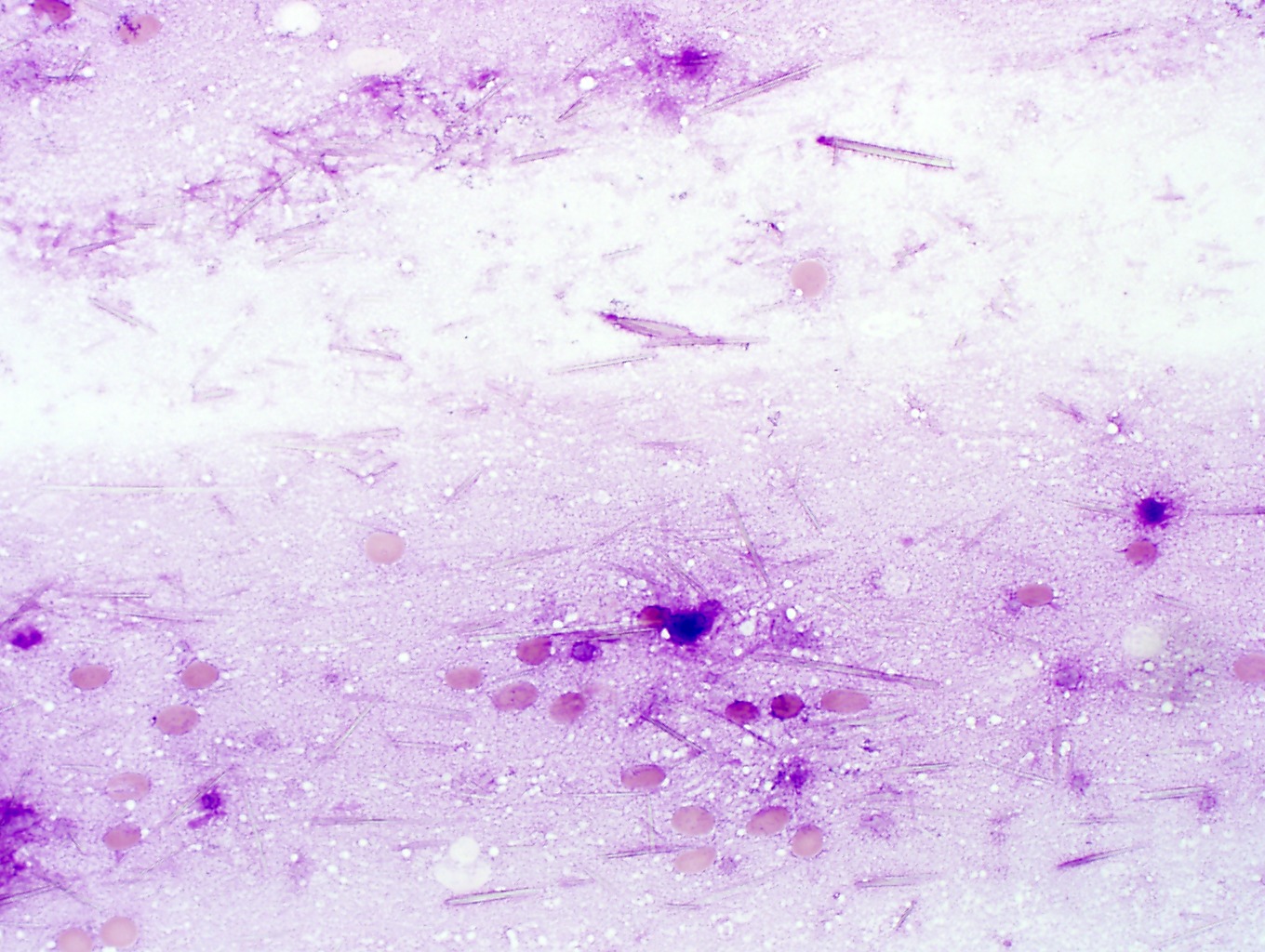
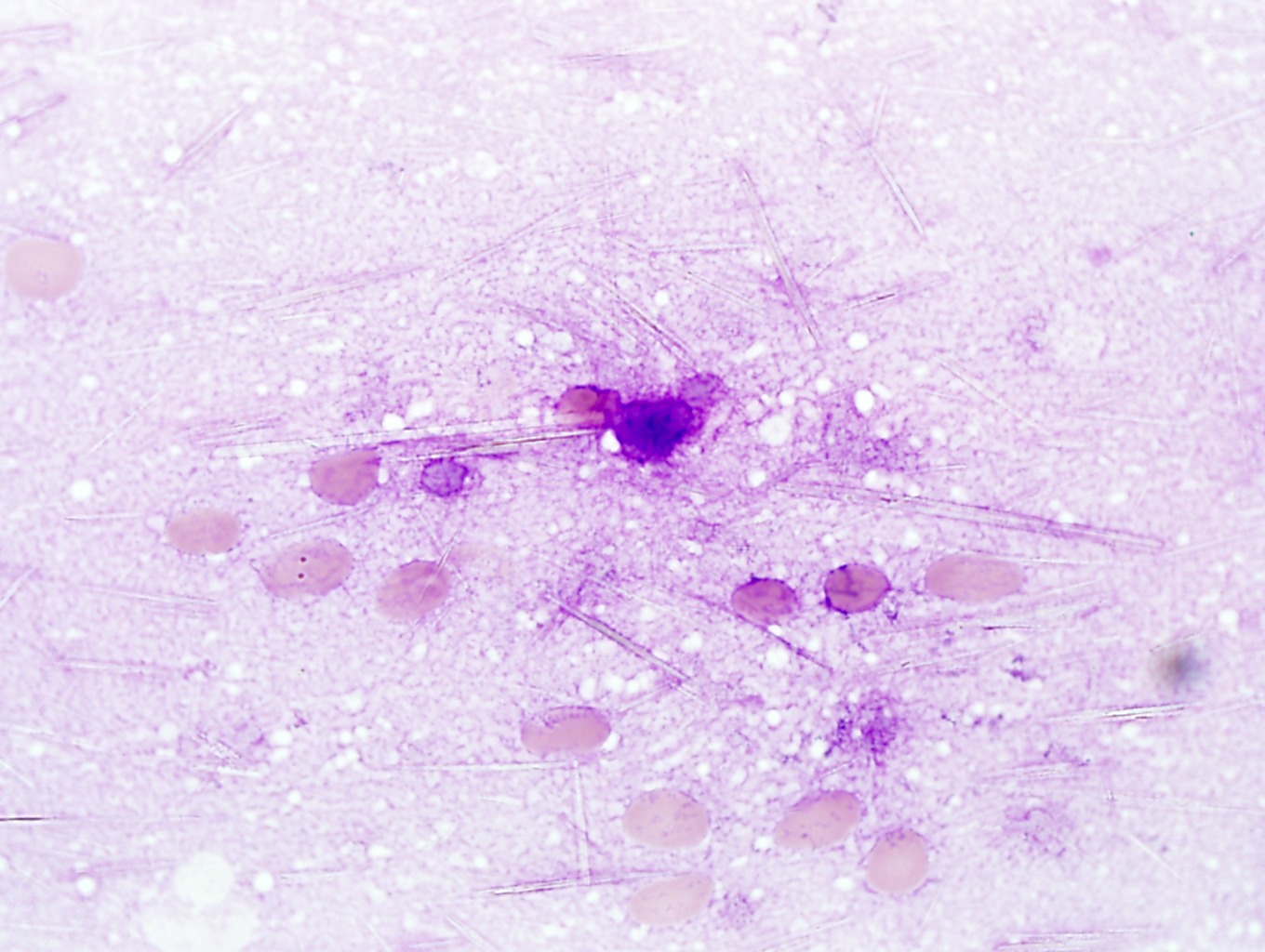
15. All synovial fluids should be examined with polarized and compensated light microscopy. Calcium pyrophosphate (pseudo-gout) crystals (A) are rhombohedral in appearance and show positive birefringence. Often you can see them with regular light microscopy within monocytic/histiocytic cells. See the arrows in Images 52, 53 and 54. Image 1-51, Image 1-52, Image 1-53, Image 1-54 Monosodium urate (urate gout) crystals (B) are needle like in appearance and show negative birefringence. Image 1-55, Image 1-56, Image 1-57 Often you will have to focus up and down to see crystals with polarized light. Although numerous neutrophils can be seen associated with gout and pseudogout, it is important to look for microorganisms which can be seen in septic joints.