Biomedical Computing
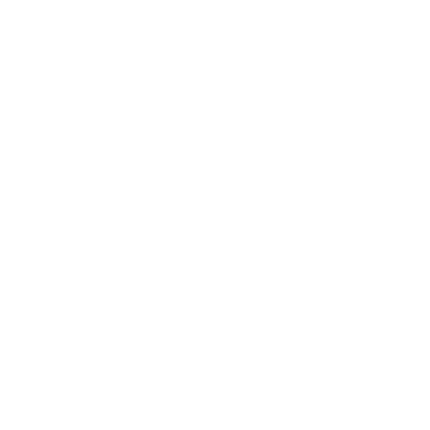
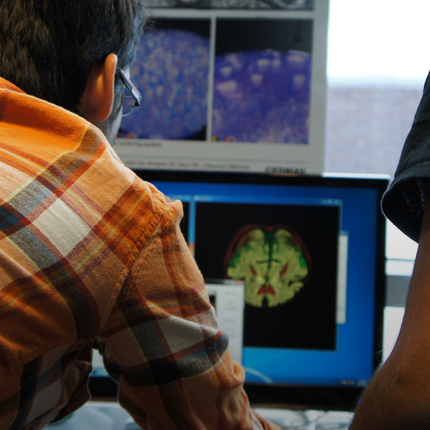
Biomedical computing combines the diagnostic and investigative aspects of biology and medical science with the power and problem-solving capabilities of modern computing. Computers are used to accelerate research learning, simulate patient behavior and visualize complex biological models.
Jeff Weiss
Computational Biomechanics
Orly Alter
Computational Biology
Tamara Bidone
Computational Models
Simulations of Biological Systems
Multi-Physics Models of Cancer Cells
Centers and Labs:
- Center for Integrative Biomedical Computing
- Muskuloskeletal Research Laboratory
- Genomic Signal Processing Lab
- Computational Biomechanics Group
Funded Research Projects:
Publications in Biomedical Computing:
 Personalized Virtual-heart Technology for Guiding the Ablation of Infarct-related Ventricular Tachycardia, A. Prakosa, H.J. Arevalo, D. Deng, P.M. Boyle, P.P. Nikolov, H. Ashikaga, J.E. Blauer, E. Ghafoori, C.J. Park, R.C. Blake III, F.T. Han, R.S. MacLeod, H.R. Halperin, D.J. Callans, R. Ranjan, J. Chrispin, S. Nazarian,, N.A. Trayanova. In Nature Biomedical Engineering, Vol. 2, pp. 732–740. 2019. DOI: doi.org/10.1038/s41551-018-0282-2 Ventricular tachycardia (VT), which can lead to sudden cardiac death, occurs frequently in patients with myocardial infarction. Catheter-based radio-frequency ablation of cardiac tissue has achieved only modest efficacy, owing to the inaccurate identification of ablation targets by current electrical mapping techniques, which can lead to extensive lesions and to a prolonged, poorly tolerated procedure. Here, we show that personalized virtual-heart technology based on cardiac imaging and computational modelling can identify optimal infarct-related VT ablation targets in retrospective animal (five swine) and human studies (21 patients), as well as in a prospective feasibility study (five patients). We first assessed, using retrospective studies (one of which included a proportion of clinical images with artefacts), the capability of the technology to determine the minimum-size ablation targets for eradicating all VTs. In the prospective study, VT sites predicted by the technology were targeted directly, without relying on prior electrical mapping. The approach could improve infarct-related VT ablation guidance, where accurate identification of patient-specific optimal targets could be achieved on a personalized virtual heart before the clinical procedure. |
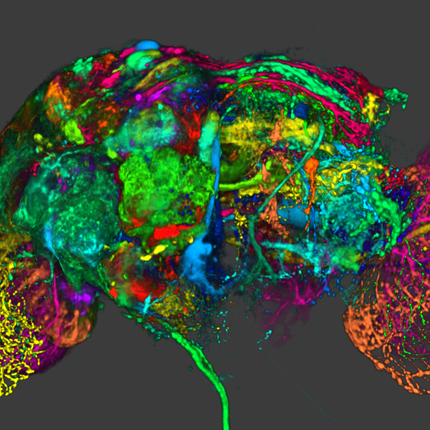
  The μDBS: Multiresolution, Directional Deep Brain Stimulation for Improved Targeting of Small Diameter Fibers D. N. Anderson, C. Anderson, N. Lanka, R. Sharma, C. R. Butson, B. W. Baker, A. D. Dorval. In Frontiers in Neuroscience, Vol. 13, October, 2019. DOI: 10.3389/fnins.2019.01152 Directional deep brain stimulation (DBS) leads have recently been approved and used in patients, and growing evidence suggests that directional contacts can increase the therapeutic window by redirecting stimulation to the target region while avoiding side-effect-inducing regions. We outline the design, fabrication, and testing of a novel directional DBS lead, theμDBS, which utilizes microscale contacts to increase the spatial resolution of stimulation steering and improve the selectivity in targeting small diameter fibers. We outline the steps of fabrication of theμDBS, from an integrated circuit design to post-processing and validation testing. We tested the onboard digital circuitry for programming fidelity, characterized impedance for a variety of electrode sizes, and demonstrated functionality in a saline bath. In a computational experiment,we determined that reduced electrode sizes focus the stimulation effect on small, nearby fibers. Smaller electrode sizes allow for a relative decrease in small-diameter axon thresholds compared to thresholds of large-diameter fibers, demonstrating a focusing of the stimulation effect within small, and possibly therapeutic, fibers. This principle of selectivity could be useful in further widening the window of therapy. TheμDBS offers a unique, multi resolution design in which any combination of microscale contacts can be used together to function as electrodes of various shapes and sizes. Multiscale electrodes could be useful in selective neural targeting for established neurological targets and in exploring novel treatment targets for new neurological indications. |
 Interactive computation and visualization of deep brain stimulation effects using Duality, J. Vorwerk, D. McCann, J. Krüger, C.R. Butson. In Computer Methods in Biomechanics and Biomedical Engineering: Imaging & Visualization, Taylor & Francis, 2019. Deep brain stimulation (DBS) is an established treatment for movement disorders such as Parkinson’s disease or essential tremor. Currently, the selection of optimal stimulation settings is performed by iteratively adjusting the stimulation parameters and is a time consuming procedure that requires multiple clinic visits of several hours. Recently, computational models to predict and visualize the effect of DBS have been developed with the goal to simplify and accelerate this procedure by providing visual guidance and such models have been made available also on mobile devices. However, currently available visualization software still either lacks mobility, i.e. it is running on desktop computers and no easily available in clinical praxis, or flexibility, as the simulations that are visualized on mobile devices have to be precomputed. The goal of the pipeline presented in this paper is to close this gap: Using Duality, a newly developed software for the interactive visualization of simulation results, we implemented a pipeline that allows to compute DBS simulations in near-real time and instantaneously visualize the result on a tablet computer. We carry out a performance analysis and present the results of a case study in which the pipeline was applied. |
  A retrospective evaluation of automated optimization of deep brain stimulation parameters J. Vorwerk, A. Brock, D.N. Anderson, J.D. Rolston, C.R. Butson. In Journal of Neural Engineering, 2019. DOI: 10.1088/1741-2552/ab35b1 Objective: We performed a retrospective analysis of an optimization algorithm for the computation of patient-specific multipolar stimulation configurations employing multiple independent current/voltage sources. We evaluated whether the obtained stimulation configurations align with clinical data and whether the optimized stimulation configurations have the potential to lead to an equal or better stimulation of the target region as manual programming, while reducing the time required for programming sessions. Methods: For three patients (five electrodes) diagnosed with essential tremor, we derived optimized multipolar stimulation configurations using an approach that is suitable for the application in clinical practice. To evaluate the automatically derived stimulation settings, we compared them to the results of the monopolar review. Results: We observe a good agreement between the findings of the monopolar review and the optimized stimulation configurations, with the algorithm assigning the maximal voltage in the optimized multipolar pattern to the contact that was found to lead to the best therapeutic effect in the clinical monopolar review in all cases. Additionally, our simulation results predict that the optimized stimulation settings lead to the activation of an equal or larger volume fraction of the target compared to the manually determined settings in all cases. Conclusions: Our results demonstrate the feasibility of an automatic determination of optimal DBS configurations and motivate a further evaluation of the applied optimization algorithm. |
  Interleaved deep brain stimulation for dyskinesia management in Parkinson's disease C. C. Aquino, G. Duffley, D. M. Hedges, J. Vorwerk, P. A. House, H. B. Ferraz, J. D. Rolston, C. R. Butson, L. E. Schrock. In Movement Disorders, 2019. DOI: 10.1002/mds.27839 Background |
 Evaluation of methodologies for computing the deep brain stimulation volume of tissue activated G. Duffley, D. N. Anderson, J. Vorwerk, A. C. Dorval, C. R. Butson. In Journal of Neural Engineering, Aug, 2019. DOI: 10.1088/1741-2552/ab3c95 Computational models are a popular tool for predicting the effects of deep brain stimulation (DBS) on neural tissue. One commonly used model, the volume of tissue activated (VTA), is computed using multiple methodologies. We quantified differences in the VTAs generated by five methodologies: the traditional axon model method, the electric field norm, and three activating function based approaches - the activating function at each grid point in the tangential direction (AF-Tan) or in the maximally activating direction (AF-3D), and the maximum activating function along the entire length of a tangential fiber (AF-Max). |
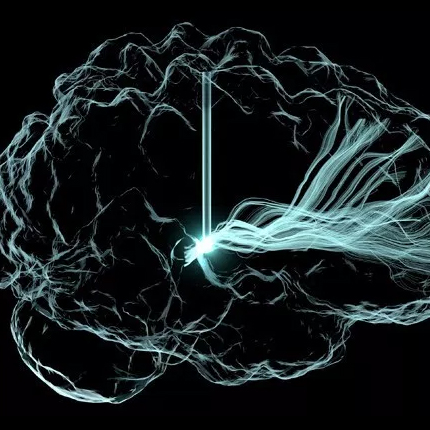
  A statistical framework for quantification and visualisation of positional uncertainty in deep brain stimulation electrodes, T. M. Athawale, K. A. Johnson, C. R. Butson, C. R. Johnson. In Computer Methods in Biomechanics and Biomedical Engineering: Imaging & Visualization, Vol. 7, No. 4, Taylor & Francis, pp. 438-449. 2019. DOI: 10.1080/21681163.2018.1523750 Deep brain stimulation (DBS) is an established therapy for treating patients with movement disorders such as Parkinson’s disease. Patient-specific computational modelling and visualisation have been shown to play a key role in surgical and therapeutic decisions for DBS. The computational models use brain imaging, such as magnetic resonance (MR) and computed tomography (CT), to determine the DBS electrode positions within the patient’s head. The finite resolution of brain imaging, however, introduces uncertainty in electrode positions. The DBS stimulation settings for optimal patient response are sensitive to the relative positioning of DBS electrodes to a specific neural substrate (white/grey matter). In our contribution, we study positional uncertainty in the DBS electrodes for imaging with finite resolution. In a three-step approach, we first derive a closed-form mathematical model characterising the geometry of the DBS electrodes. Second, we devise a statistical framework for quantifying the uncertainty in the positional attributes of the DBS electrodes, namely the direction of longitudinal axis and the contact-centre positions at subvoxel levels. The statistical framework leverages the analytical model derived in step one and a Bayesian probabilistic model for uncertainty quantification. Finally, the uncertainty in contact-centre positions is interactively visualised through volume rendering and isosurfacing techniques. We demonstrate the efficacy of our contribution through experiments on synthetic and real datasets. We show that the spatial variations in true electrode positions are significant for finite resolution imaging, and interactive visualisation can be instrumental in exploring probabilistic positional variations in the DBS lead. |
  Image-based analysis and long-term clinical outcomes of deep brain stimulation for Tourette syndrome: a multisite study K. A. Johnson, P. T. Fletcher, D. Servello, A. Bona, M. Porta, J. L. Ostrem, E. Bardinet, M. Welter, A. M. Lozano, J. C. Baldermann, J. Kuhn, D. Huys, T. Foltynie, M. Hariz, E. M. Joyce, L. Zrinzo, Z. Kefalopoulou, J. Zhang, F. Meng, C. Zhang, Z. Ling, X. Xu, X. Yu, A. YJM Smeets, L. Ackermans, V. Visser-Vandewalle, A. Y. Mogilner, M. H. Pourfar, L. Almeida, A. Gunduz, W. Hu, K. D. Foote, M. S. Okun, C. R. Butson. In Journal of Neurology, Neurosurgery & Psychiatry, BMJ Publishing Group, 2019. DOI: 10.1136/jnnp-2019-320379 BACKGROUND: METHODS:
We collected retrospective clinical data and imaging from 13 international sites on 123 patients. We assessed the effects of DBS over time in 110 patients who were implanted in the centromedial (CM) thalamus (n=51), globus pallidus internus (GPi) (n=47), nucleus accumbens/anterior limb of the internal capsule (n=4) or a combination of targets (n=8). Contact locations (n=70 patients) and volumes of tissue activated (n=63 patients) were coregistered to create probabilistic stimulation atlases.RESULTS:
Tics and obsessive-compulsive behaviour (OCB) significantly improved over time (p<0.01), and there were no significant differences across brain targets (p>0.05). The median time was 13 months to reach a 40% improvement in tics, and there were no significant differences across targets (p=0.84), presence of OCB (p=0.09) or age at implantation (p=0.08). Active contacts were generally clustered near the target nuclei, with some variability that may reflect differences in targeting protocols, lead models and contact configurations. There were regions within and surrounding GPi and CM thalamus that improved tics for some patients but were ineffective for others. Regions within, superior or medial to GPi were associated with a greater improvement in OCB than regions inferior to GPi.CONCLUSION:
The results collectively indicate that DBS may improve tics and OCB, the effects may develop over several months, and stimulation locations relative to structural anatomy alone may not predict response. This study was the first to visualise and evaluate the regions of stimulation across a large cohort of patients with TS to generate new hypotheses about potential targets for improving tics and comorbidities.
|
  Neural Selectivity, Efficiency, and Dose Equivalence in Deep Brain Stimulation through Pulse Width Tuning and Segmented Electrodes C.J. Anderson, D.N. Anderson, S.M. Pulst, C.R. Butson, A.D. Dorval. In bioRxiv, Cold Spring Harbor Laboratory, April, 2019. DOI: 10.1101/613133 Background |
  Anodic stimulation misunderstood: preferential activation of fiber orientations with anodic waveforms in deep brain stimulation D.N. Anderson, G. Duffley, J. Vorwerk, A.D. Dorval, C.R. Butson. In Journal of Neural Engineering, Vol. 16, No. 1, IOP Publishing, pp. 016026. Jan, 2019. DOI: 10.1088/1741-2552/aae590 Objective. During deep brain stimulation (DBS), it is well understood that extracellular cathodic stimulation can cause activation of passing axons. Activation can be predicted from the second derivative of the electric potential along an axon, which depends on axonal orientation with respect to the stimulation source. We hypothesize that fiber orientation influences activation thresholds and that fiber orientations can be selectively targeted with DBS waveforms. Approach. We used bioelectric field and multicompartment NEURON models to explore preferential activation based on fiber orientation during monopolar or bipolar stimulation. Preferential fiber orientation was extracted from the principal eigenvectors and eigenvalues of the Hessian matrix of the electric potential. We tested cathodic, anodic, and charge-balanced pulses to target neurons based on fiber orientation in general and clinical scenarios. Main results. Axons passing the DBS lead have positive second derivatives around a cathode, whereas orthogonal axons have positive second derivatives around an anode, as indicated by the Hessian. Multicompartment NEURON models confirm that passing fibers are activated by cathodic stimulation, and orthogonal fibers are activated by anodic stimulation. Additionally, orthogonal axons have lower thresholds compared to passing axons. In a clinical scenario, fiber pathways associated with therapeutic benefit can be targeted with anodic stimulation at 50% lower stimulation amplitudes. Significance. Fiber orientations can be selectively targeted with simple changes to the stimulus waveform. Anodic stimulation preferentially activates orthogonal fibers, approaching or leaving the electrode, at lower thresholds for similar therapeutic benefit in DBS with decreased power consumption. |
  A High-Resolution Head and Brain Computer Model for Forward and Inverse EEG Simulation A. Warner, J. Tate, B. Burton,, C.R. Johnson. In bioRxiv, Cold Spring Harbor Laboratory, Feb, 2019. DOI: 10.1101/552190 To conduct computational forward and inverse EEG studies of brain electrical activity, researchers must construct realistic head and brain computer models, which is both challenging and time consuming. The availability of realistic head models and corresponding imaging data is limited in terms of imaging modalities and patient diversity. In this paper, we describe a detailed head modeling pipeline and provide a high-resolution, multimodal, open-source, female head and brain model. The modeling pipeline specifically outlines image acquisition, preprocessing, registration, and segmentation; three-dimensional tetrahedral mesh generation; finite element EEG simulations; and visualization of the model and simulation results. The dataset includes both functional and structural images and EEG recordings from two high-resolution electrode configurations. The intermediate results and software components are also included in the dataset to facilitate modifications to the pipeline. This project will contribute to neuroscience research by providing a high-quality dataset that can be used for a variety of applications and a computational pipeline that may help researchers construct new head models more efficiently. |
  Anodic Stimulation Misunderstood: Preferential Activation of Fiber Orientations with Anodic Waveforms in Deep Brain Stimulation D. N. Anderson, G. Duffley, J. Vorwerk, A. Dorval, C. R. Butson. In Journal of Neural Engineering, IOP Publishing, Oct, 2018. DOI: 10.1088/1741-2552/aae590 Objective: During deep brain stimulation (DBS), it is well understood that extracellular cathodic stimulation can cause activation of passing axons. Activation can be predicted from the second derivative of the electric potential along an axon, which depends on axonal orientation with respect to the stimulation source. We hypothesize that fiber orientation influences activation thresholds and that fiber orientations can be selectively targeted with DBS waveforms. Approach: We used bioelectric field and multicompartment NEURON models to explore preferential activation based on fiber orientation during monopolar or bipolar stimulation. Preferential fiber orientation was extracted from the principal eigenvectors and eigenvalues of the Hessian matrix of the electric potential. We tested cathodic, anodic, and charge-balanced pulses to target neurons based on fiber orientation in general and clinical scenarios. Main Results: Axons passing the DBS lead have positive second derivatives around a cathode, whereas orthogonal axons have positive second derivatives around an anode, as indicated by the Hessian. Multicompartment NEURON models confirm that passing fibers are activated by cathodic stimulation, and orthogonal fibers are activated by anodic stimulation. Additionally, orthogonal axons have lower thresholds compared to passing axons. In a clinical scenario, fiber pathways associated with therapeutic benefit can be targeted with anodic stimulation at 50% lower stimulation amplitudes. Significance: Fiber orientations can be selectively targeted with simple changes to the stimulus waveform. Anodic stimulation preferentially activates orthogonal fibers, approaching or leaving the electrode, at lower thresholds for similar therapeutic benefit in DBS with decreased power consumption. |
  Mathematically universal and biologically consistent astrocytoma genotype encodes for transformation and predicts survival phenotype K. A. Aiello, S. P. Ponnapalli, O. Alter. In APL Bioengineering, Vol. 2, No. 3, AIP Publishing, pp. 031909. September, 2018. DOI: 10.1063/1.5037882 DNA alterations have been observed in astrocytoma for decades. A copy-number genotype predictive of a survival phenotype was only discovered by using the generalized singular value decomposition (GSVD) formulated as a comparative spectral decomposition. Here, we use the GSVD to compare whole-genome sequencing (WGS) profiles of patient-matched astrocytoma and normal DNA. First, the GSVD uncovers a genome-wide pattern of copy-number alterations, which is bounded by patterns recently uncovered by the GSVDs of microarray-profiled patient-matched glioblastoma (GBM) and, separately, lower-grade astrocytoma and normal genomes. Like the microarray patterns, the WGS pattern is correlated with an approximately one-year median survival time. By filling in gaps in the microarray patterns, the WGS pattern reveals that this biologically consistent genotype encodes for transformation via the Notch together with the Ras and Shh pathways. Second, like the GSVDs of the microarray profiles, the GSVD of the WGS profiles separates the tumor-exclusive pattern from normal copy-number variations and experimental inconsistencies. These include the WGS technology-specific effects of guanine-cytosine content variations across the genomes that are correlated with experimental batches. Third, by identifying the biologically consistent phenotype among the WGS-profiled tumors, the GBM pattern proves to be a technology-independent predictor of survival and response to chemotherapy and radiation, statistically better than the patient's age and tumor's grade, the best other indicators, and MGMT promoter methylation and IDH1 mutation. We conclude that by using the complex structure of the data, comparative spectral decompositions underlie a mathematically universal description of the genotype-phenotype relations in cancer that other methods miss. |
  Validation and Opportunities of Electrocardiographic Imaging: From Technical Achievements to Clinical Applications M. Cluitmans, D. H. Brooks, R. MacLeod, O. Dössel, M. S. Guillem, P. M. van Dam, J. Svehlikova, B. He, J. Sapp, L. Wang, L. Bear. In Frontiers in Physiology, Vol. 9, Frontiers Media SA, pp. 1305. 2018. ISSN: 1664-042X DOI: 10.3389/fphys.2018.01305 Electrocardiographic imaging (ECGI) reconstructs the electrical activity of the heart from a dense array of body-surface electrocardiograms and a patient-specific heart-torso geometry. Depending on how it is formulated, ECGI allows the reconstruction of the activation and recovery sequence of the heart, the origin of premature beats or tachycardia, the anchors/hotspots of re-entrant arrhythmias and other electrophysiological quantities of interest. Importantly, these quantities are directly and noninvasively reconstructed in a digitized model of the patient’s three-dimensional heart, which has led to clinical interest in ECGI’s ability to personalize diagnosis and guide therapy. |
 Personalized virtual-heart technology for guiding the ablation of infarct-related ventricular tachycardia, A. Prakosa, H. J. Arevalo, D. Deng, P. M. Boyle, P. P. Nikolov, H. Ashikaga, J. J. E. Blauer, E. Ghafoori, C. J. Park, R. C. Blake, F. T. Han, R. S. MacLeod, H. R. Halperin, D. J. Callans, R. Ranjan, J. Chrispin, S. Nazarian, N. A. Trayanova. In Nature Biomedical Engineering, Springer Nature America, Inc, September, 2018. DOI: 10.1038/s41551-018-0282-2 Ventricular tachycardia (VT), which can lead to sudden cardiac death, occurs frequently in patients with myocardial infarction. Catheter-based radio-frequency ablation of cardiac tissue has achieved only modest efficacy, owing to the inaccurate identification of ablation targets by current electrical mapping techniques, which can lead to extensive lesions and to a prolonged, poorly tolerated procedure. Here, we show that personalized virtual-heart technology based on cardiac imaging and computational modelling can identify optimal infarct-related VT ablation targets in retrospective animal (five swine) and human studies (21 patients), as well as in a prospective feasibility study (five patients). We first assessed, using retrospective studies (one of which included a proportion of clinical images with artefacts), the capability of the technology to determine the minimum-size ablation targets for eradicating all VTs. In the prospective study, VT sites predicted by the technology were targeted directly, without relying on prior electrical mapping. The approach could improve infarct-related VT ablation guidance, where accurate identification of patient-specific optimal targets could be achieved on a personalized virtual heart before the clinical procedure. |
  Fully Automatic Left Atrium Segmentation from Late Gadolinium Enhanced Magnetic Resonance Imaging Using a Dual Fully Convolutional Neural Network Z. Xiong, V. V. Fedorov, X. Fu, E. Cheng, R. Macleod, J. Zhao. In IEEE Transactions on Medical Imaging, IEEE, pp. 1--1. 2018. DOI: 10.1109/tmi.2018.2866845 Atrial fibrillation (AF) is the most prevalent form of cardiac arrhythmia. Current treatments for AF remain suboptimal due to a lack of understanding of the underlying atrial structures that directly sustain AF. Existing approaches for analyzing atrial structures in 3D, especially from late gadolinium-enhanced (LGE)-MRIs, rely heavily on manual segmentation methods which are extremely labor-intensive and prone to errors. As a result, a robust and automated method for analyzing atrial structures in 3D is of high interest. We have therefore developed AtriaNet, a 16-layer convolutional neural network (CNN), on 154 3D LGE-MRIs with a spatial resolution of 0.625 mm × 0.625 mm × 1.25 mm from patients with AF, to automatically segment the left atrial (LA) epicardium and endocardium. AtriaNet consists of a multi-scaled, dual pathway architecture that captures both the local atrial tissue geometry, and the global positional information of LA using 13 successive convolutions, and 3 further convolutions for merging. By utilizing computationally efficient batch prediction, AtriaNet was able to successfully process each 3D LGE-MRI within one minute. Furthermore, benchmarking experiments showed that AtriaNet outperformed state-of-the-art CNNs, with a DICE score of 0.940 and 0.942 for the LA epicardium and endocardium respectively, and an inter-patient variance of <0.001. The estimated LA diameter and volume computed from the automatic segmentations were accurate to within 1.59 mm and 4.01 cm³ of the ground truths. Our proposed CNN was tested on the largest known dataset for LA segmentation, and to the best of our knowledge, it is the most robust approach that has ever been developed for segmenting LGE-MRIs. The increased accuracy of atrial reconstruction and analysis could potentially improve the understanding and treatment of AF. |
  Deep brain stimulation for the treatment of disorders of consciousness and cognition in traumatic brain injury patients: a review B. Kundu, A. A. Brock, D. J. Englot, C. R. Butson, J. D. Rolston. In Neurosurgical Focus, Vol. 45, No. 2, Journal of Neurosurgery Publishing Group (JNSPG), pp. E14. Aug, 2018. DOI: 10.3171/2018.5.focus18168 Traumatic brain injury (TBI) is a looming epidemic, growing most rapidly in the elderly population. Some of the most devastating sequelae of TBI are related to depressed levels of consciousness (e.g., coma, minimally conscious state) or deficits in executive function. To date, pharmacological and rehabilitative therapies to treat these sequelae are limited. Deep brain stimulation (DBS) has been used to treat a number of pathologies, including Parkinson disease, essential tremor, and epilepsy. Animal and clinical research shows that targets addressing depressed levels of consciousness include components of the ascending reticular activating system and areas of the thalamus. Targets for improving executive function are more varied and include areas that modulate attention and memory, such as the frontal and prefrontal cortex, fornix, nucleus accumbens, internal capsule, thalamus, and some brainstem nuclei. The authors review the literature addressing the use of DBS to treat higher-order cognitive dysfunction and disorders of consciousness in TBI patients, while also offering suggestions on directions for future research. |
  Targeting Neuronal Fiber Tracts for Deep Brain Stimulation Therapy Using Interactive, Patient-Specific Models, A. Janson, C. Butson. In Journal of Visualized Experiments, No. 138, MyJove Corporation, Aug, 2018. DOI: 10.3791/57292 Deep brain stimulation (DBS), which involves insertion of an electrode to deliver stimulation to a localized brain region, is an established therapy for movement disorders and is being applied to a growing number of disorders. Computational modeling has been successfully used to predict the clinical effects of DBS; however, there is a need for novel modeling techniques to keep pace with the growing complexity of DBS devices. These models also need to generate predictions quickly and accurately. The goal of this project is to develop an image processing pipeline to incorporate structural magnetic resonance imaging (MRI) and diffusion weighted imaging (DWI) into an interactive, patient specific model to simulate the effects of DBS. A virtual DBS lead can be placed inside of the patient model, along with active contacts and stimulation settings, where changes in lead position or orientation generate a new finite element mesh and solution of the bioelectric field problem in near real-time, a timespan of approximately 10 seconds. This system also enables the simulation of multiple leads in close proximity to allow for current steering by varying anodes and cathodes on different leads. The techniques presented in this paper reduce the burden of generating and using computational models while providing meaningful feedback about the effects of electrode position, electrode design, and stimulation configurations to researchers or clinicians who may not be modeling experts. |